Irritable bowel syndrome (IBS) is a common condition that influences the large intestine, and affects about 11,2 people worldwide.
It is a chronic long-term disorder that causes symptoms such as bloating, gas, cramping, abdominal pain, and diarrhea or constipation, or sometimes even both. But the symptoms are severe only for a few people.
Some people can manage their moderate symptoms by IBS diet, changes in lifestyle and relieving stress. More-severe IBS can usually be treated with counseling and medication.
It has to be said that IBD and IBS are not the same. Despite similar acronyms and symptoms, these two disorders are extremely different. Here’s why:
- IBD is an umbrella term that represents two autoimmune conditions (ulcerative colitis and Crohn’s disease) that cause inflammation or destruction in the lining of the intestines wall, which may lead to sores and narrowing of the bowels.
- IBS is a condition of the gastrointestinal (GI) tract, and it doesn’t lead to changes in bowel tissue. Also, it does not increase your risk of colorectal cancer. Some people may have both IBD as well as IBS.
Researchers are still not sure about the causes of this gut disorder, but it might be a combination of several factors, such as sensitive gastrointestinal tract, stress, changes in gut microbes and hormones (1, 7).
Finding a suitable treatment that helps may take time, but there’s a lot you can try. Here in this article you`ll find many lifestyle and diet tips for IBS, so you could learn to manage IBS naturally.
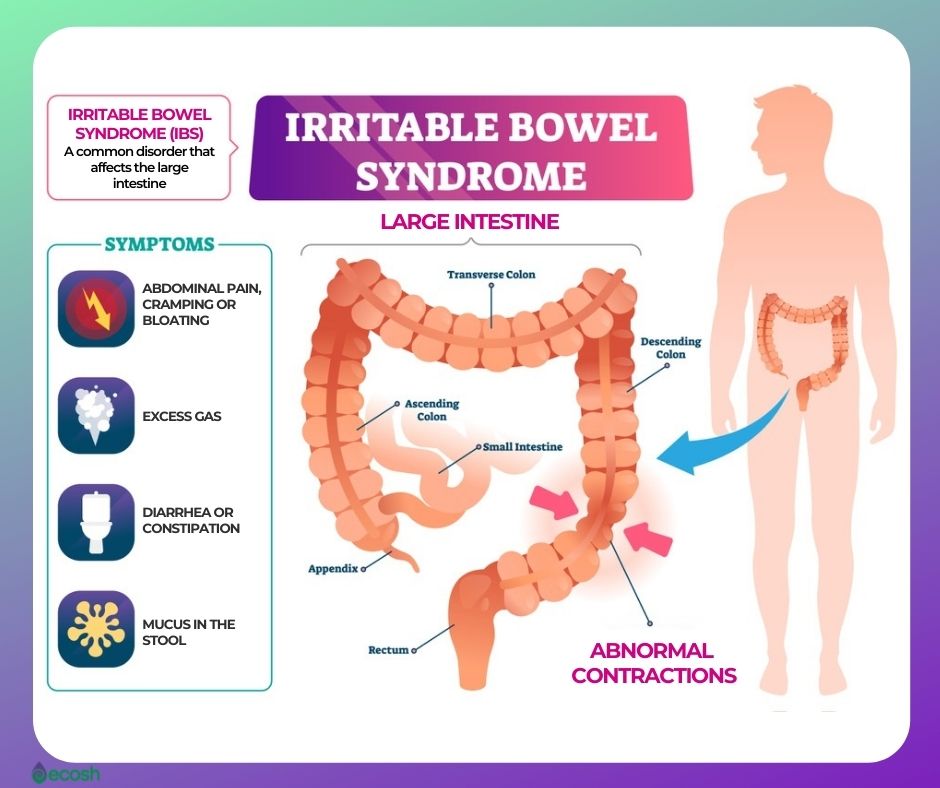
Irritable Bowel Syndrome (IBS) Symptoms and Signs
The symptoms of irritable bowel syndrome may differ, but commonly exist for a long time. There may be times when your symptoms are better (remissions) and times when they’re worse (flare-ups). They may be triggered by food or drink.
The most usual IBS symptoms include:
- Abdominal pain or cramps that are associated with passing a bowel movement. In other words, the pain or cramping is usually worse after eating and better after doing poo.
- Changes in the frequency and appearance of bowel movement.
- Bloating. Meaning, your stomach may feel swollen and uncomfortably full.
- Diarrhea. You may sometimes need to poop suddenly or have watery poo.
- Constipation. You may feel like you cannot empty your bowels fully, or you may strain when pooping.
Other symptoms of IBS include:
- Increased gas and farting (flatulence)
- Bowel incontinence. It means you may not always be able to control when you poop
- Mucus in the stool
- Lack of energy and tiredness
- Nausea (feeling sick)
- Backache
- Problems peeing, such as:
Consult your doctor if you have a continuous change in bowel movements or other symptoms of IBS. If you have more-serious symptoms such as weight loss, diarrhea at night, iron deficiency anemia, rectal bleeding, unexplained vomiting, persistent pain that isn’t relieved by passing gas or a bowel movement or difficulty swallowing consult your doctor, as they may indicate a more serious condition, such as colon cancer (1).
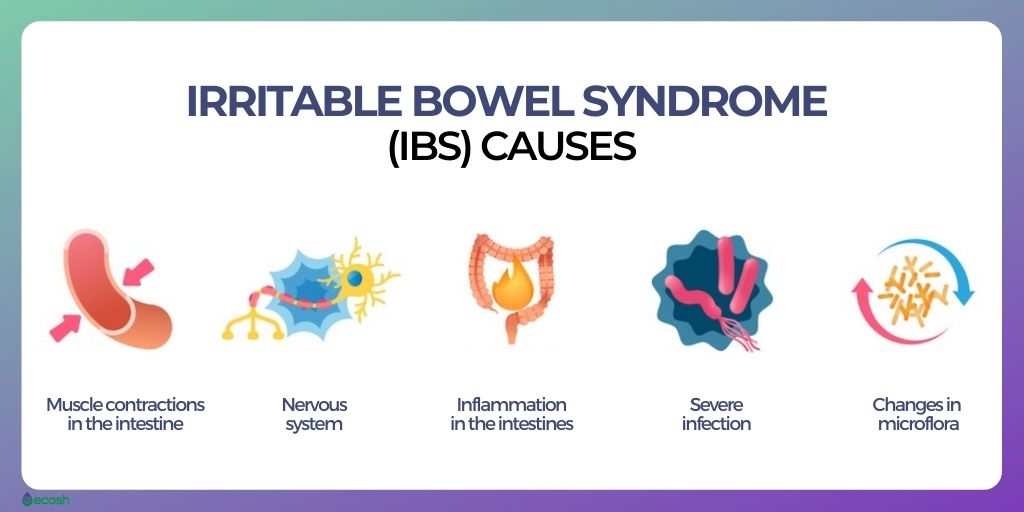
Irritable Bowel Syndrome (IBS) Causes – What Causes IBS?
The precise causes of IBS are still not known. However, researchers do have a few theories about factors that seem to play a role:
- More sensitive colon than normally.
- Abnormal muscle contractions in the intestine:
- Contractions of muscles that line the walls of the intestines that last longer and are stronger than normal can cause bloating, gas and diarrhea.
- While weaker bowel contractions can slow down food passage and cause dry and hard stools.
- Abnormal nervous system. In people with IBS, the brain may perceive contractions in the gut more sensitively than in others, and cause your body to overreact to changes that normally happen in the digestive process. This may result in pain, diarrhea or constipation.
- Severe infection. A severe diarrhea (gastroenteritis) or bout caused by bacteria or a virus may also lead to IBS.
- Bacterial overgrowth. IBS might also be caused by a surplus of bacteria in the intestines.
- Stress. Individuals who have suffered from stressful events, particularly in childhood, seem to have more symptoms of IBS.
- Changed gut microbes. The microbes, such as for example bacteria, fungi and viruses, which normally live in the intestines and play a key role in health – might be different in people with IBS.
- Immune system. The immune system reaction to stress and infection may be different in people with IBS.
- Hormones. As 70% of those who suffer from IBS are women, it is suspected that hormonal changes may also trigger IBS symptoms.
- Serotonin levels. The neurotransmitter serotonin (produced in the gut) may have an impact on digestive tract nerves:
- People with diarrhea-predominant IBS may have increased serotonin amounts in the gut.
- People with constipation-predominant IBS may have decreased serotonin levels (1, 3).

IBS Triggers – How do I Know What Triggers IBS and How to Learn Avoid Triggering IBS?
Symptoms and flare-ups of IBS can be promoted by:
Diet. Although the role of food allergy or intolerance in IBS isn’t fully understood, diet seems to play a huge role in triggering IBS as many people have worse IBS symptoms after drinking or eating specific drinks or foods.
- Constipation-predominant IBS can be triggered by certain foods that can make IBS-related constipation worse. These foods include:
- Dairy products, particularly cheese
- Cereals and breads made with refined (not whole) grains
- Processed foods like cookies and chips
- Coffee, alcohol and carbonated drinks
- High-protein diets
- Diarrhea-predominant IBS can also be triggered by certain foods that can make IBS-related diarrhea worse. These foods include:
- Too large meals
- Fatty and fried foods
- Carbonated beverages
- Too much fiber, particularly the insoluble fiber contained in the skin of vegetables and fruits
- Food and drinks that contain caffeine, chocolate, alcohol, sorbitol, or fructose
- Dairy products, particularly in people with lactose intolerance (can’t digest the milk sugar lactose)
- Foods with wheat for people with gluten intolerance
- Constipation-predominant IBS can be triggered by certain foods that can make IBS-related constipation worse. These foods include:
Stress and anxiety. Majority of people with IBS undergo worse or more-frequent symptoms during periods of increased stress or anxiety. However, stress may only aggravate symptoms, it doesn’t cause them. Stress can come from a lot of sources, including:
- Problems at home or with family
- Work
- Your commute
- Money issues
- A feeling that everything is out of your control
Certain drugs. People with IBS may have trouble with certain drugs that can trigger IBS related constipation or diarrhea such as:
- Certain antidepressants
- Antibiotics
- Medications made with sorbitol, such as for example cough syrup
Menstrual cycle. Women with IBS seem to experience more severe symptoms during their periods.
Other triggers such as:

Types of IBS
- IBS-C. IBS with constipation, or constipation-predominant IBS, or IBS-C, is one of the most common types of IBS.
- IBS-D. IBS with diarrhea or diarrhea-predominant IBS, or IBS-D is the opposite to constipation-predominant IBS.
- IBS-M or IBS-A. IBS-M or also called IBS-A is inflammatory bowel syndrome with mixed bowel habits, meaning with alternating constipation and diarrhea.
- Post-infectious IBS or PI-IBS. This is a condition in which the symptoms of IBS (mostly diarrhea) occur after you’ve had a GI infection.
- Post-diverticulitis IBS. This type of IBS in which the symptoms are similar to PI-IBS – is just one possible complication after having diverticulitis that has been treated. Diverticulitis happens when the small pouches that line the lower part of your large intestine (diverticula) get inflamed or infected (6).
Irritable Bowel Syndrome (IBS) Risk Groups and Risk Factors – Who is at Risk For IBS?
Many people may have periodic symptoms of irritable bowel syndrome, but it does not mean that they have IBS. The risk factors that seem to make some people more likely to have this syndrome than others include:
- Age. Although IBS can affect people of all ages, it occurs more frequently in people in their teens and under age 50.
- Gender. This condition is more frequent among women, as about twice as many women as men have IBS. It’s not exactly known why, but some scientists suspect the changing hormones in the menstrual cycle may have a role in it. Estrogen treatment during menopause may also be a risk factor for inflammatory bowel syndrome.
- Genes. IBS seems to run in families.
- Stress and emotional problems. Anxiety, depression or other mental health disorders seem to play a role in developing IBS. Having been through a traumatic event in life such as a history of emotional, sexual or physical violence also might be a risk factor.
- Medications. According to studies there is a link between IBS symptoms and antidepressants, antibiotics, as well as medications made with sorbitol.
- Food sensitivities and intolerance. Although there’s no evidence that specific foods can cause IBS, some foods may certainly trigger the symptoms. Some people may have gastrointestinal systems that are sensitive to wheat, dairy, the sugar substitute sorbitol, or a sugar in fruits (fructose). Certain other foods and beverages such as fatty foods, alcohol, and carbonated drinks may also disturb digestion. In addition, wrong eating habits like eating large meals, or eating while you do something stressful can also cause trouble with digestion.
- Other problems with digestion. Some researchers think that illnesses such as stomach flu, traveler’s diarrhea or food poisoning may trigger a person’s first IBS symptoms. PI IBS happens in about up to 32 percent of people who’ve had a gastrointestinal infection, a bout of acute stomach flu. Symptoms like abdominal discomfort and diarrhea can last 2-3 years (1, 3).

Irritable Bowel Syndrome (IBS) Complications
Although IBS may lead to complications, none of these are luckily life-threatening. Irritable bowel syndrome does not cause cancer or other more severe bowel-related diseases. Some of the health problems IBS may cause include:
- Hemorrhoids. Chronic constipation or diarrhea may cause swollen blood vessels around your anus, which can bleed and hurt.
- Impacted bowel (a fecal impaction). Long term constipation may lead to stool blockage in your colon and cause pain, headache, nausea, and vomiting. It mostly occurs with older adults. Consult your doctor immediately if you have signs this may be happening.
- Poor quality of life. Flare-ups can occur unexpectedly and not being able to predict how you’ll feel may negatively affect the quality of your life. According to research, individuals with IBS miss three times as many days from work as do people without IBS.
- Mood disorders, depression and anxiety. As there is a link between your brain and gut, undergoing symptoms of IBS may lead to depression or anxiety which in turn also can make IBS symptoms worse.
- Malnourishment. Avoiding certain foods can relieve your IBS symptoms. However, in this case your body may not get all the vitamins and nutrients it needs.
- Pregnancy complications. Hormonal changes as well as the pressure a baby puts on the bowel wall may lead to more severe digestive issues. Many women also choose to stop any IBS drugs they’re taking during pregnancy, as this can be better for the baby. However, it can make moms-to-be more likely to have things like indigestion and heartburn (1, 3).
Irritable Bowel Syndrome (IBS) Treatment – Medications, Lifestyle Changes, Home Remedies, Alternative Medicine, IBS Diet, Low FODMAP Diet and Supplements for IBS
Treatment of IBS mostly concerns relieving symptoms so that IBS patients could enjoy life without constant worry and live as normally as possible. See your doctor to diagnose IBS and find the suitable treatment together.
Medications for IBS
Medications specially for IBS. As some of the IBS medications may have serious side effects, doctors usually prescribe these only when other treatment has not worked. Medicines that are specifically for IBS treatment and are approved for some people with irritable bowel syndrome include:
- Alosetron (Lotronex)
- Eluxadoline (Viberzi)
- Rifaximin (Xifaxan)
- Lubiprostone (Amitiza)
- Linaclotide (Linzess)
Antidepressants. As IBS may lead to mood problems and depression, your doctor may recommend antidepressants.
- Tricyclic antidepressants. These medicines (imipramine, desipramine or nortriptyline) – which may be prescribed even if you have abdominal pain and diarrhea without depression – can also help alleviate depression and hold back the action of neurons that control the intestines to help reduce pain.
- Selective serotonin reuptake inhibitor (SSRI) antidepressants. These medications, such as fluoxetine or paroxetine, may also be helpful if you have pain and constipation or you are depressed.
Other medications. Based on your symptoms your doctor might suggest medications such as:
- Anti-diarrheal medications. Some OTC medicines, such as loperamide or a bile acid binder may help control diarrhea. However, bile acid binders may cause bloating.
- Anticholinergic medications. Medicines like dicyclomine can help relieve painful bowel spasms, and are sometimes prescribed for people who have bouts of diarrhea. These drugs are usually safe but may cause dry mouth, blurred vision and constipation.
- Pain medications. Gabapentin and pregabalin may relieve severe bloating or pain.
Supplements and laxatives for IBS. Your doctor may also recommend you certain supplements such as:
- Fiber supplements. In case of constipation you may find help from psyllium supplements with fluids.
- Laxatives. If fiber doesn’t relieve your constipation, your doctor may suggest certain OTC (over-the-counter) laxatives (1).

Lifestyle Changes, Home Remedies and Alternative Medicine for IBS
You can often control your modest signs and symptoms by making changes in your diet and lifestyle and by managing stress. Here are some suggestions for IBS relief you can try:
- Follow the IBS diet or FODMAP diet and avoid eating problem foods that may trigger your symptoms (see the full list below).
- Get enough sleep. Not sleeping enough puts your body into stress. Therefore, sleeping at least 7-8 hours a day is vital for you. If you have sleeping disorders or you suffer from insomnia, you can try practicing good sleep hygiene or take natural supplements for insomnia.
- Eat at regular times each day and do not skip meals. Eating about the same time every day helps to regulate bowel function.
- Reduce stress. Experiencing stress may make IBS worse. Therefore it’s very important to learn to manage your stress. Try yoga, meditation or whatever soothes your mind. There are very simple yoga poses for stress that can be truly helpful.
- Mindfulness and breathing exercises. Lessening your stress by practicing breathing exercises and mindfulness may also be helpful in calming down the misfiring gut nerves.
- Exercise regularly. It’s a well known fact that exercise helps lessen stress and depression, but it also stimulates normal contractions of your intestines.
- Hypnosis. Hypnosis can be effective for IBS as it can lessen abdominal pain and bloating. However, you cannot do it alone and need a trained professional who teaches you how to enter a relaxed state and then guides you in relaxing your abdominal muscles.
- Acupuncture. With IBS-C (constipation-predominant IBS), acupuncture may help relax the autonomic nervous system, which helps balance your GI tract. Acupuncture may even help people with IBS-D.
- Peppermint oil pill. According to studies, in people who have diarrhea-predominant IBS, a specifically coated pill that slowly releases peppermint oil (enteric-coated peppermint oil) in the small intestine eases urgency, bloating, pain while passing stool and abdominal pain.
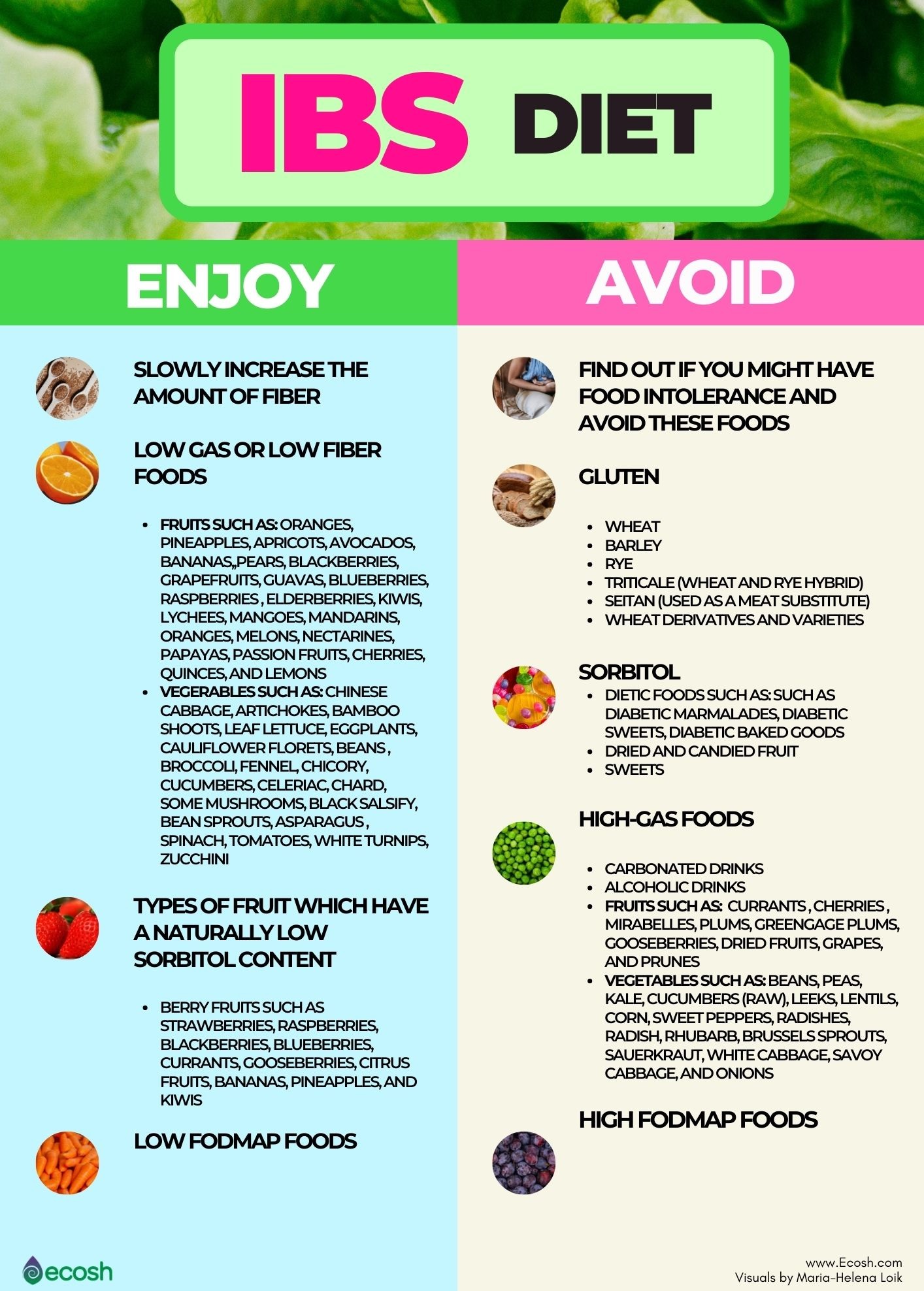
IBS Diet
Meal planning and general diet suggestions for IBS
- Drink plenty of plain water during the day.
- Eat at regular times each day and try to not skip meals. Eating about the same time every day helps to regulate bowel function.
- In case of diarrhea, eating small, frequent meals may make you feel better.
- In case of constipation, eating larger amounts of fiber-rich foods may help move food through your intestines.
Foods that can make IBS symptoms worse and should be limited or avoided in case IBS
Find out if you might have food intolerance. Firstly, you should avoid these foods to which you are intolerant as these can make your IBS symptoms worse. However, these foods can be different for everyone.
- Some people with IBS may feel better when they avoid dairy, wheat, coffee, yeast, eggs, citrus fruits and potatoes.
- Also sugars and fats can make diarrhea more severe.
High-fiber foods. Although fiber usually helps relieve constipation, it also can aggravate gas and cramping. Therefore, it is best to slowly increase the amount of fiber in your daily menu over a period of weeks.
- Little by little boost your fiber intake by 2 to 3 grams per day until you’re consuming 25 grams (women) or 38 grams (men) per day. Foods that contain fiber include beans, whole grains (also whole-grain bread and cereals), fruits, and vegetables.
- You can try ground flaxseed. For instance, sprinkle it on cooked vegetables or salads.
- However, a fiber supplement might be a better choice, as it may cause less bloating and gas than high-fiber foods. It activates the intestinal peristalsis, accelerates the progression of food, and induces a faster sense of a full stomach. In addition, fibers purify gut walls by binding and excreting toxins, residues, and excess cholesterol. Consuming the required amount of fiber daily helps to prevent many health problems such as obesity, irritable bowel syndrome, heart disease, diabetes, and kidney stones.
Avoid high-gas foods. If you experience gas or bloating, you might want to avoid foods and beverages that may lead to increased gas. These foods and drinks to avoid include:
- Carbonated beverages
- Alcoholic beverages
- Fruits that cause severe gas include currants (red and black), cherries (sweet and sour), mirabelles, plums, greengage plums, gooseberries, dried fruit (raisins, apricots, figs, etc.), grapes, and prunes
- Vegetables that cause severe gas include beans, peas, kale, cucumbers (raw), leeks, lentils, corn, sweet peppers, radishes, radish, rhubarb, Brussels sprouts, sauerkraut, white cabbage, savoy cabbage, and onions
Avoid sorbitol. Avoid or eat only a moderate amount of foods that contain the sugar substitute sorbitol, such as:
- Dietetic foods such as diabetic marmalades, diabetic sweets, diabetic baked goods
- Fruits which have a naturally high sorbitol content such as apples, pears, cherries, prunes, plums, dates fruits with seeds, such as mirabelles, apricots, nectarines, and all fruit syrups made from these types of fruits
- Sorbitol is used as a coating for dried and candied fruit such as sultanas, raisins, plums and dried fruit
- Sorbitol in sweets such as chewing gum, jelly babies, jelly fruits, candies, chocolate bars, filled wafers, chocolate, etc.
- It is also added to some dry products in order to maintain a smooth consistency, for instance, semolina, pudding powder, pudding sugar, etc. Although, it is there in very small amounts (4).
Avoid gluten. According to research, some individuals with IBS report improvement in diarrhea symptoms if they stop eating gluten even if they don’t have celiac disease. Foods that contain gluten include:
- Wheat
- Barley
- Rye
- Triticale (wheat and rye hybrid)
- Seitan (used as a meat substitute)
- Wheat derivatives and varieties such as: spelt, durum, couscous, semolina, farina, farro, kamut, einkorn, wheat berries, bulgur, wheat bran, wheat starch, wheat germ, emmer, and graham flour.
Avoid high FODMAP foods. IBS patients may also find help in following a low FODMAP diet. Read more about low FODMAP foods to eat and high FODMAP foods to avoid below in section Low FODMAP Diet For Inflammatory Bowel Disease (IBS).
Suitable foods for IBS that are easily digestible
- Fruits that cause little gas or are low in fiber and easily digestible include: oranges, pineapples, apricots, avocados, bananas, figs (fresh), pears, blackberries, strawberries, grapefruits, guavas, blueberries, raspberries , elderberries, kiwis, lychees, mangoes, mandarins, oranges, melons (cantaloupe, watermelons, honey melons), nectarines, papayas, passion fruits, cherries, cranberries, quinces, and lemons.
- Vegetables that cause little gas or are low in fiber and easily digestible include: chinese cabbage, artichokes, bamboo shoots, leaf lettuce (iceberg, red lettuce, mache, Batavia lettuce, etc.), eggplants, cauliflower florets, beans (green, fine), broccoli, fennel, chicory, cucumbers (cooked), celeriac, chard, mushrooms (button mushrooms, forest mushrooms, chanterelles), black salsify, bean sprouts, asparagus (green or white), spinach, celery, Teltow turnips, tomatoes, white turnips, and zucchini.
- Types of fruit which have a naturally low sorbitol content include berry fruits such as strawberries, raspberries, blackberries, blueberries, currants, gooseberries, citrus fruits, bananas, pineapples, and kiwis
- Low FODMAP foods (see below) (4).
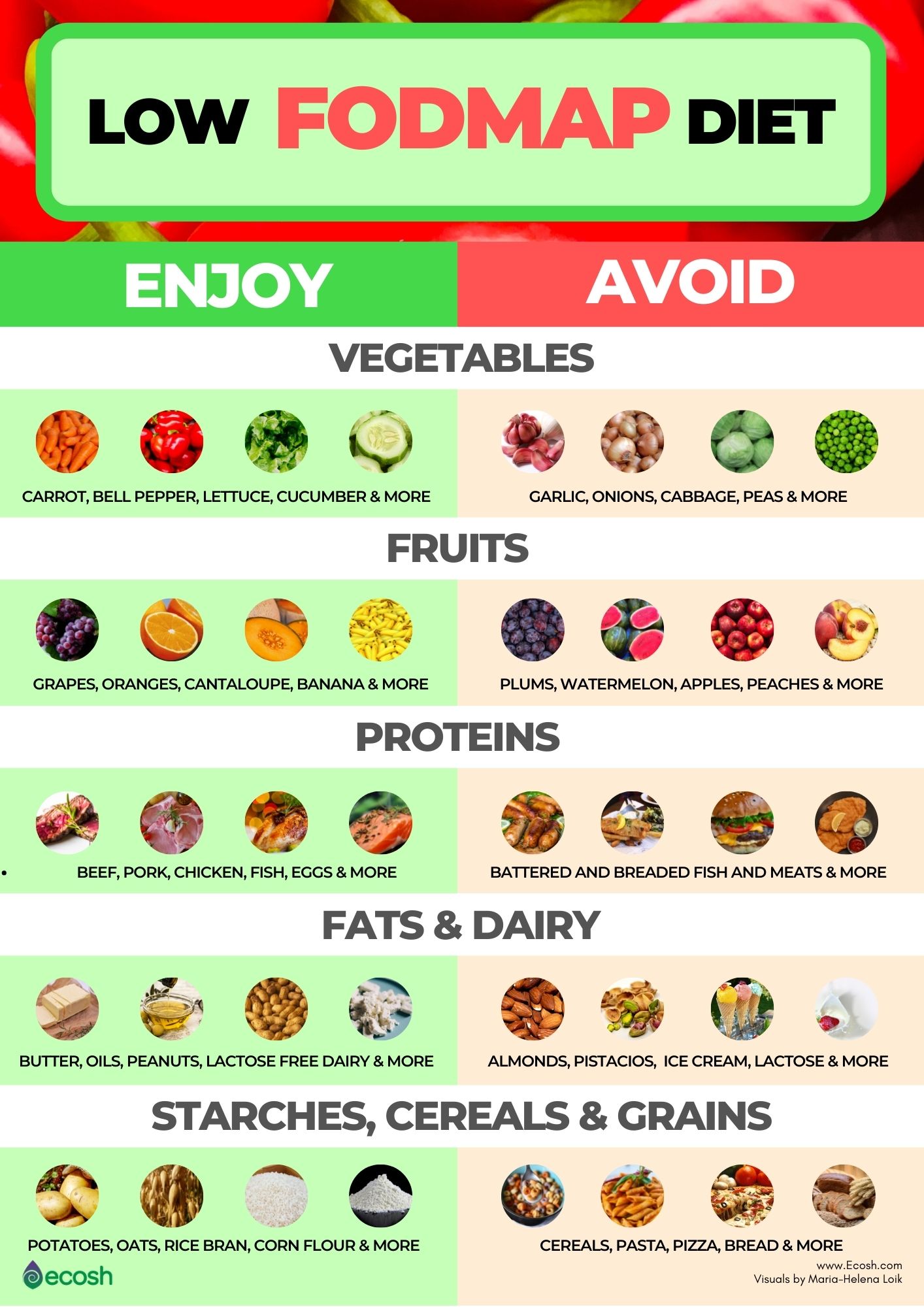
Low FODMAP Diet For Inflammatory Bowel Disease (IBS)
Your doctor may suggest you try a FODMAP (Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols) diet to cut out some carbohydrates that are hard to digest.
These are sugar alcohols and short-chain carbohydrates that your body absorbs poorly. Therefore, eating a lot of FODMAP foods may cause abdominal pain, gas, abdominal distention, bloating and diarrhea.
This diet plan may be difficult to follow, as it cuts out many common foods that may contain high FODMAP foods. Certain foods are totally eliminated or extremely limited for 3-8 weeks, then gradually reintroduced into a low-FODMAP diet to see if they cause symptoms (elimination diet). It is not meant to be a permanent solution because it is very restrictive, but it may work well enough to be a treatment for people with gastrointestinal (GI) problems.
Sometimes also portion sizes can make a difference, because if you eat only extremely small amounts, there might not be enough high FODMAPs to cause you symptoms. However, it is advisable to contact your health care professional or a dietitian to make sure that you are on the right track and getting enough dietary nutrients that you can consume.
The Three Phases of The Low FODMAP Diet – Elimination Phase, Reintroduction Phase and Integration Phase
So, let’s thoroughly explain the low FODMAP diet phases.
Low FODMAP diet phases:
- Elimination phase
- Reintroduction phase
- Integration phase
Step 1. FODMAP Elimination Phase (2-6 weeks)
- Goal: The goal of elimination phase is to identify the high FODMAP foods from your present daily menu that you commonly consume, and that are provoking your IBS symptoms or symptoms of some other health condition.
- How to implement?: Firstly, see the list of the high FODMAP foods below, and switch them out for low FODMAP alternatives.
- How long does it take and when can I expect the results?: Some people start to feel better as early as after two days. However, for others, noticing results can take a few weeks. So, be patient! Overall, how long you spend time in the elimination phase should be set on in consultation with your healthcare professional, but estimatedly and usually it lasts about 2-6 weeks.
- Can I cheat in the elimination phase?: No! You should not have any cheating moments when implementing this diet. Because if you stick to it with your full commitment, the more accurate and effective the results are. Therefore, stay strong! For instance, if you are used to eating apples, swap your daily high FODMAP apple for a low FODMAP strawberries or orange.
Step 2. FODMAP Reintroduction Phase (6-8 weeks)
- Goal: The goal of the reintroduction phase is to determine which high-FODMAP foods trigger symptoms and which do not.
- How to implement?: In this phase you gradually (one by one) reintroduce single high-FODMAP foods back into your diet. If a specific food does not cause any symptoms then you can include that specific food into your daily diet from now on. However, if it does cause symptoms – you should eliminate this food permanently.
- It’s important to remember that you should reintroduce every FODMAP subgroup (Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols) one by one while the rest of the diet remains low in FODMAPs. Sticking to this method allows you to see which FODMAP subgroups you may have intolerances to. Otherwise it will be impossible to understand what foods trigger your symptoms and all the effort goes to waste.
- How long does it take and when can I expect the results?: Usually it can take about 6 to 8 weeks to finally find out all your trigger foods. If a certain food is not suitable, you should notice it immediately or within a few days. Therefore, do not rush the process and take a break for a few days between the reintroduction of single foods, as otherwise there can be crossover effects.
This step can be the most tricky and hard to implement for people, therefore consult your healthcare professional if you need any help.
Step 3: FODMAP Integration Phase (Lifelong)
- Goal: The goal of the integration phase is to establish your personalized and persistent FODMAP diet.
- How to implement?: After finding out foods that you tolerate and foods that are triggering your symptoms, you can start reintroducing FODMAPs that you were able to tolerate well and avoid only those FODMAPSs that set off your symptoms (11).

Low FODMAP foods on a low FODMAP diet include:
- Vegetables such as: alfalfa sprouts, carrot, bell pepper, bean sprouts, bok choy, green beans, lettuce, cucumber, tomato, zucchini, eggplant, bamboo shoots, ginger, olives, chives, potatoes, parsnips, and turnips.
- Fresh fruits such as: grapes, oranges, cantaloupe, banana, honeydew melon, blueberries, kiwi, grapefruit, lemon, strawberries, and lime.
- Dairy that is lactose-free, and hard cheeses, or ripened/matured cheeses such as feta cheese, camembert and brie. However, if you are not lactose intolerant, you may not need to avoid dairy with lactose.
- Beef, pork, chicken, fish, eggs.
- Soy products including tempeh and tofu.
- Grains such as: oats, oat bran, rice, rice bran, corn flour, quinoa, sourdough spelled bread, gluten-free bread and pasta (although gluten is not a FODMAP, many gluten-free products tend to be low in FODMAPs).
- Non-dairy milk such as: almond milk, coconut milk, and rice milk.
- Drinks such as: tea and coffee (use non-dairy milk or creamers).
- Fruit juice not from concentrate.
- Fats such as butter (butter is considered low FODMAP food, because the amount of lactose per serving is 1 gram or less) and oils.
- Water.
- Nuts such as: peanuts, walnuts, macadamia and pine nuts (fewer than 10-15/serving for nuts).
- Seeds such as: pumpkin seeds (1, 5, 10).

High FODMAP foods that you should avoid include:
- Breadcrumbs, marinades, and sauces/gravies that may be high in FODMAPs.
- Vegetables such as: garlic, onions, cabbage, broccoli, snow peas, cauliflower, asparagus, leeks, artichokes, beetroot, sweet corn, celery, brussels sprouts.
- Mushrooms.
- Fruits such as (particularly “stone” fruits): apricots, peaches, plums, nectarines, prunes, mangoes, pears, apples, cherries, watermelon, avocados and blackberries.
- Sausages, battered fish and breaded meats and fish.
- Dried fruits and fruit juice concentrate.
- Beans and lentils.
- Wheat and rye products such as: cereals, pasta, pizza, bread, and crackers.
- Dairy products that contain lactose such as: ice cream, milk, soft cheese, yogurt, cottage cheese, and pudding.
- Nuts, such as cashews, almonds and pistachios.
- Sweeteners and artificial sweeteners such as: sorbitol, mannitol, maltitol, xylitol, agave nectar, honey, high fructose corn syrup and isomalt (usually found in sugar-free mints and gums, and also cough syrups).
- Drinks such as: coconut water, sports drinks and alcohol (1, 5).
Supplements for IBS
Supplements that may ease IBS symptoms include include:
- Probiotics. Good bacteria, also called probiotics, are live bacteria and yeasts that are good for you, especially for your digestive system. These good bacteria normally live in your intestines and are found in certain foods, such as buttermilk, yogurt, sauerkraut and in dietary supplements. According to recent studies, some probiotics may also ease IBS symptoms, such as bloating, diarrhea and abdominal pain.
- Fiber supplements. In case of constipation-predominant IBS you may find help from fiber supplements that contain psyllium.
- L-Glutamine. According to study, oral glutamine supplements may safely lessen all major IBS-related symptoms (1, 9).
Some Important Facts About IBS
- No one fully knows what causes IBS.
- Doctors do not think that in IBS it’s “all in your head”.
- IBS is not a cancer and will not lead to cancer.
- IBS is not an anatomical health problem.
- It is not a recognizable physical or chemical disorder.
- It will not lead to other gastrointestinal (GI) diseases (3).
NB! The information provided here is for informational purposes only, so do not consider it as health care or medical diagnosis and treatment. Do not consider this information as a guarantee of the results you want to achieve. In addition, this information is not intended to replace the advice of your physician or other healthcare professional.
Even more, you should not use it to diagnose or treat a health problem. Before taking any dietary supplements or changing or discontinuing your existing medication, treatment, or care, be sure to consult with your healthcare professional or doctor before starting any diet or program, or if you suspect you may have a medical condition.
Written by Maria-Helena Loik
Pictures: Pexels.com, Pixabay.com, Shutterstock.com
Sources:
- Irritable bowel syndrome – Diagnosis and treatment – Mayo Clinic
- Symptoms – Irritable bowel syndrome NHS (www.nhs.uk)
- Irritable Bowel Syndrome (IBS) Causes of IBS (webmd.com)
- sorbit_intolerance.indd (gastroenterologie-ffm.de)
- Low FODMAP Diet for IBS: List of Foods to Eat and Avoid (medicinenet.com)
- Types of IBS: Symptoms, Diagnosis & Treatment (healthline.com)
- Irritable bowel syndrome: prevalence, risk factors in an adult Lebanese population | BMC Gastroenterology | Full Text (biomedcentral.com)
- 7 Natural Remedies for IBS | Everyday Health
- Randomised placebo-controlled trial of dietary glutamine supplements for postinfectious irritable bowel syndrome | Gut (bmj.com)
- Is butter lactose-free? And is butter low FODMAP? | Butter & Lactose (karlijnskitchen.com)
- Phases of the FODMAP diet explained – Canadian Digestive Health Foundation (cdhf.ca)


