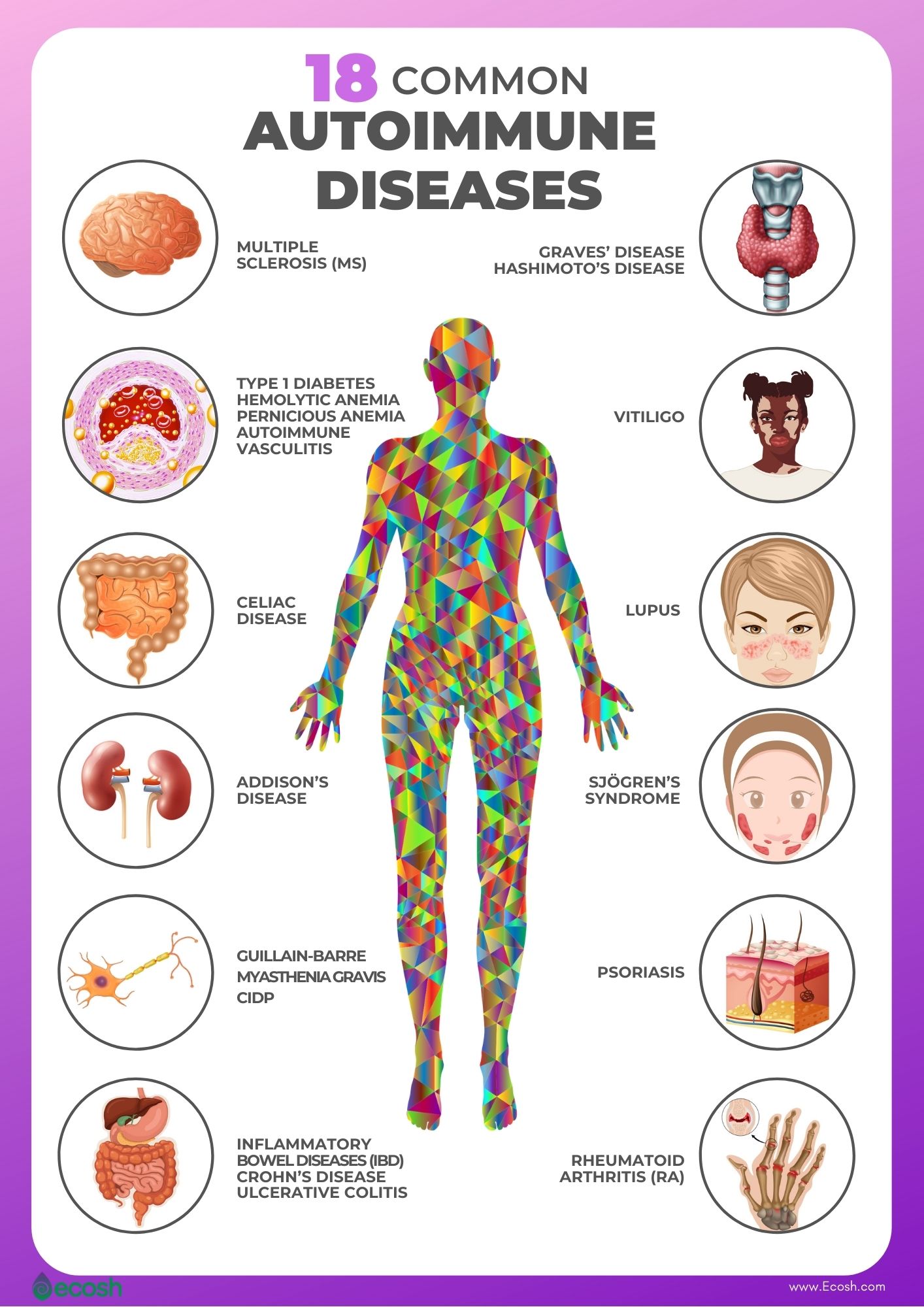
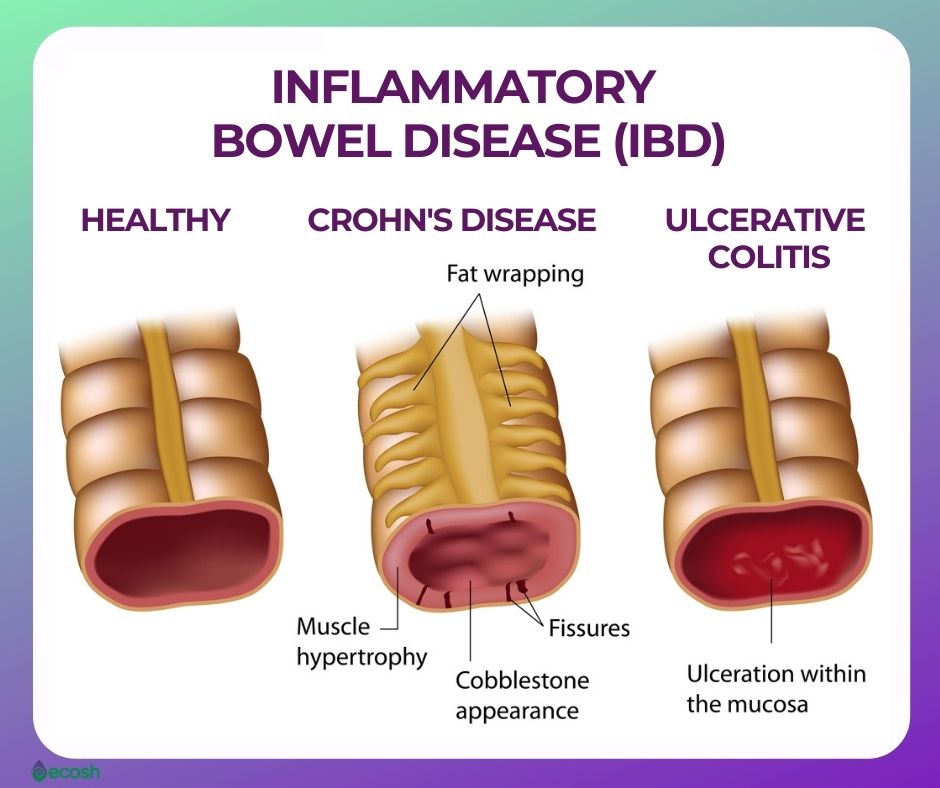
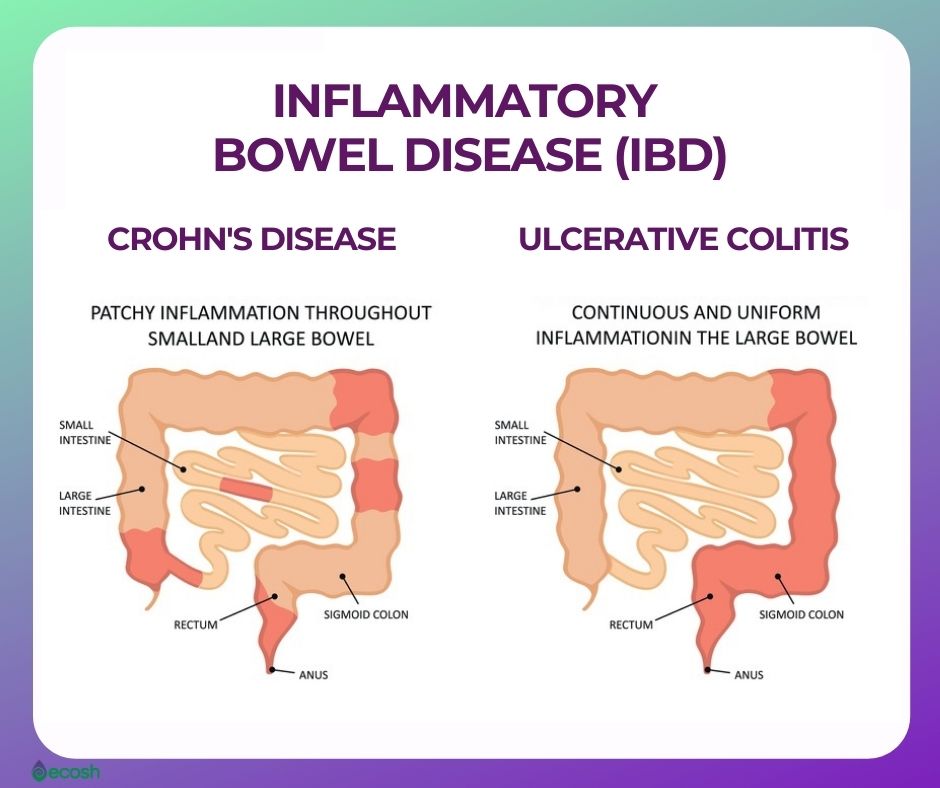
Crohn’s disease is an autoimmune disorder, a type of an inflammatory bowel disease (IBD). Inflammatory bowel disease (IBD) is an umbrella term that represents two conditions that cause inflammation in the lining of the intestinal wall. Each type of IBD affects a different part of the gastrointestinal (GI) tract.
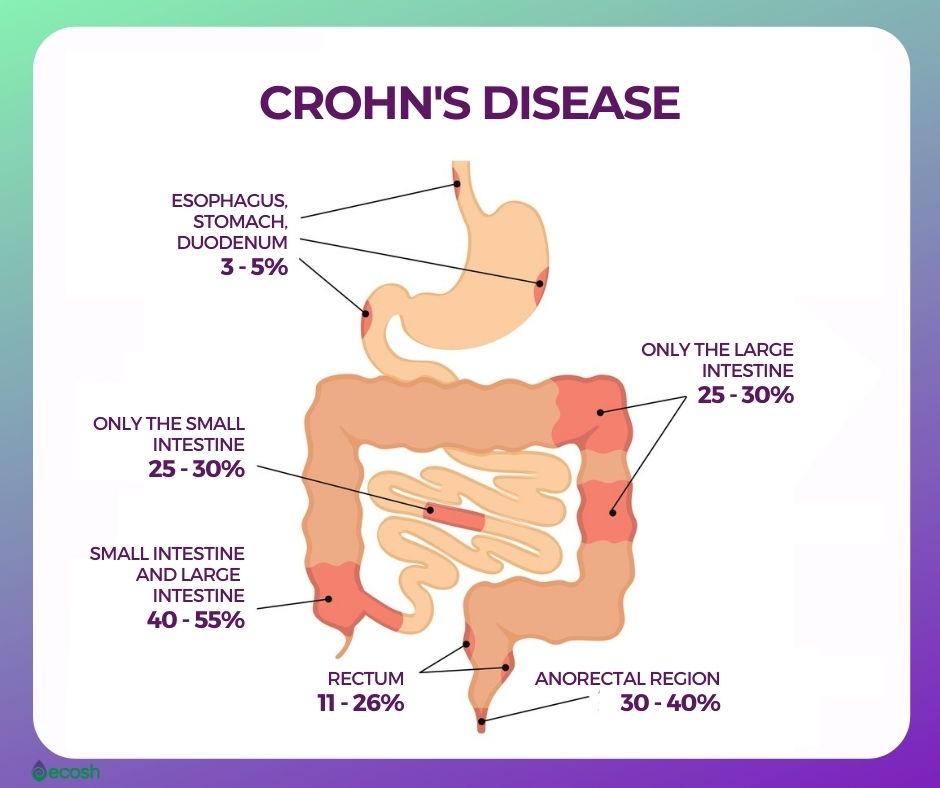
- Crohn’s disease can affect any part of the gastrointestinal (GI) tract, from the mouth to the anus. This chronic disease causes inflammation of the digestive tract, which can involve different areas of the digestive tract in different people, and lead to malnutrition, abdominal pain, fatigue, severe diarrhea, and weight loss. Crohn’s disease can be weakening as well as painful, and it may sometimes lead to life-threatening complications.
- Ulcerative colitis. This disorder influences only the lining of the large intestine (colon) and rectum.
Crohn’s disease affects mostly individuals in western Europe and North America, where it has a prevalence of 100 to 300 per 100,000 people.
Although there’s no known cure for Crohn’s disease, some therapies and medications can significantly lessen its signs and symptoms and even bring healing of inflammation and long-term remission. With treatment, the right diet and nutrition, many people with Crohn’s disease are able to function well (1, 3).
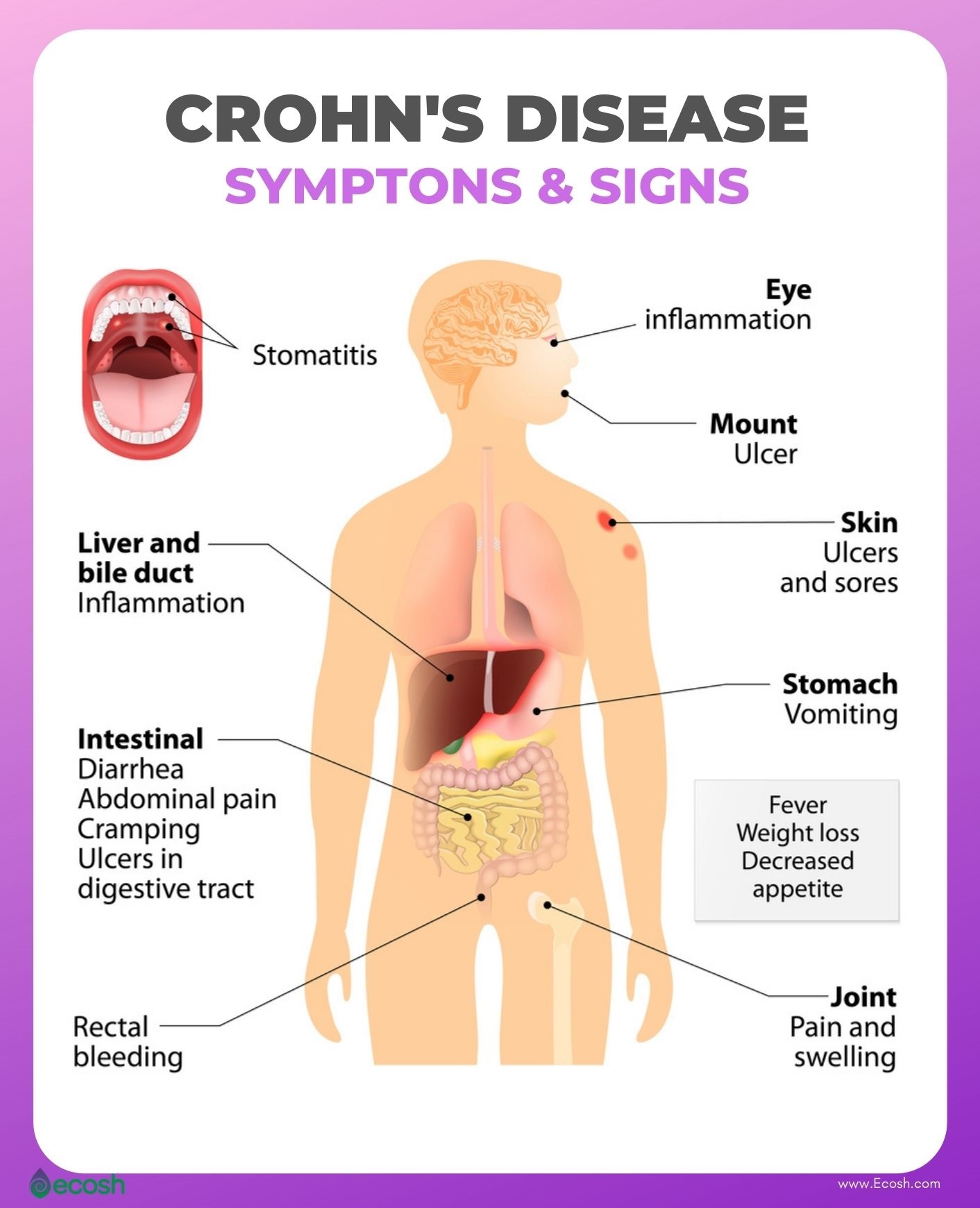
Crohn’s Disease Symptoms and Signs
Symptoms and signs of Crohn’s disease can vary from mild to severe, and usually develop gradually. However, sometimes symptoms may come on suddenly, without warning. You may experience periods of time when you have no signs or symptoms (remission), or times when symptoms suddenly reactivate (flare-ups).
This disorder may influence any part of the gastrointestinal tract, from your mouth to your anus. In some patients, the disorder affects only the colon (part of the large intestine). Although symptoms range from person to person, there are some common symptoms of inflammation of the GI tract caused by Crohn’s disease. See your doctor if you have any symptoms of Crohn’s disease or persistent changes in your bowel habits (1).
When the Crohn’s disease is in its active form, signs and symptoms may include:
- Persistent diarrhea
- Urgent need to move bowels
- Sensation of incomplete bowel evacuation
- Fever
- Fatigue
- Abdominal pain and cramps
- Rectal bleeding
- Blood in your stool
- Mouth sores
- Reduced appetite
- Unexplained weight loss
- Drainage or pain around or near the anus because of inflammation from a tunnel into the skin (fistula)
- Constipation, which can lead to bowel obstruction (1, 2).
In case severe Crohn’s disease, people may also experience symptoms such as:
- Iron deficiency (anemia)
- Inflammation of eyes, skin and joints
- Inflammation of the liver or bile ducts
- Kidney stones
- In children, delayed growth or sexual development (1).
Crohn’s Disease Causes
The immune system normally guards against germs like bacteria, viruses, fungi, and other microorganisms. When it detects these alien invaders, it sends out an army of fighter cells to attack them.
Normally, the immune system can tell the difference between foreign cells and your own cells and during a normal immune response, cells travel out of the blood to the intestines and produce inflammation. Under normal circumstances, harmless bacteria that’s present in the gastrointestinal tract are protected from an immune system attack.
However, in an autoimmune disease like Crohn’s disease, the harmless bacteria are mistaken for foreign invaders, and an abnormal immune response causes the immune system to attack the cells in the digestive tract, too. The Immune response causes the inflammation which does not go away. This leads to chronic inflammation, ulceration, thickening of the intestinal wall, and, eventually, symptoms of Crohn’s disease.
The precise causes of Crohn’s disease are not yet well understood. Earlier, doctors suspected that diet and stress were the culprits, however now it`s known that these factors may aggravate Crohn’s disease, but don’t cause it. According to recent research, several factors, such as heredity, genetics, environmental factors, and a malfunctioning immune system, may contribute to its development.
Also, although scientists have not proved it yet, it’s possible that bacterium or a virus may be the trigger of Crohn’s disease (1,2).
Crohn’s Disease Risk factors and Risk Groups
Risk factors and risk groups for Crohn’s disease may include:
Age. The disorder can occur at any age, however Crohn’s disease is most frequent when you’re young, between the ages of 15 and 35.
Gender. Women and men are both equally likely to be affected.
Ethnicity. Crohn’s disease may affect any ethnic group, however the condition is more common among white people, particularly people of Eastern European backgrounds, including Jews of European descent (Ashkenazi). Though, there have been an increased number of cases reported in African-American populations who live in North America and the United Kingdom in recent years.
Geography and environment. Crohn’s disease is more common:
- Northern climates, rather than southern climates
- In developed countries, rather than undeveloped countries
- Urban cities and towns, rather than rural areas
Genetics and heredity. As Crohn’s disease tends to run in families, you’re at higher risk of developing the disease if you have a first-degree relative with this condition. According to studies, between 5% and 20% of people with irritable bowel syndrome (IBD) have a family member, such as a parent, child, or sibling, who also has one of the diseases. The genetic risk is higher with Crohn’s disease than ulcerative colitis. However, most Crohn’s disease patients don’t have family members with the disease.
Cigarette smoking. Smoking may increase the likelihood of developing Crohn’s disease, and make Crohn’s more severe. Research suggests that women who smoke are at higher risk to develop Crohn’s Disease, and need surgery, than men who smoke.
Nonsteroidal anti-inflammatory medications. Although some medications such as for example naproxen sodium (Aleve), ibuprofen (Advil, Motrin IB, others), diclofenac sodium and others, are not the causes of Crohn’s disease, they can make Crohn’s disease worse, as they may lead to inflammation of the bowel (1, 2, 4).
Crohn’s Disease Complications
Crohn’s disease may cause one or more complications such as:
Malnutrition. Often people with Crohn’s disease develop anemia due to low vitamin B-12 or iron. It’s because abdominal pain, cramping and diarrhea may make it hard to eat or for your intestine to absorb the necessary amount of nutrients to keep you nourished.
Bowel obstruction. Some parts of the bowel can scar and narrow, which may block the flow of digestive contents. Therefore, over time, Crohn’s disease can influence the whole thickness of the intestinal wall. People with Crohn’s disease may need surgery to remove the diseased part of the bowel.
Ulcers. Chronic and lasting inflammation due to Crohn’s disease may cause ulcers (open sores) everywhere in the digestive tract, including in the genital area (perineum), anus and mouth.
Fistulas. Occasionally ulcers can extend entirely through the intestinal wall, and create an unnatural connection between different body parts – a fistula. Fistulas may evolve between your skin and intestine, or between another organ and your intestine. The most common kind of fistulas are Fistulas near or around the anal area (perianal). In case fistulas form in the abdomen, food may bypass areas of the bowel that are necessary for absorption. Fistulas may develop in the bladder or vagina, between loops of bowel, or through the skin, causing constant drainage of bowel contents to your skin. Sometimes, a fistula may become infected and form an abscess, which can be life-threatening without treatment.
Anal fissure. Anal fissure is a small rip in the tissue that lines the anus or in the skin around the anus where infections can happen. It’s frequently linked with painful bowel movements and may lead to a perianal fistula.
Blood clots. This disorder increases the likelihood of developing blood clots in arteries and veins.
Colon cancer. Crohn’s disease that influences your colon increases your likelihood of developing colon cancer.
Other health problems. Crohn’s disease may also lead to other conditions, such as for example anemia, gallbladder or liver disease, osteoporosis, skin disorders, and arthritis.
Medicine risks:
- Some Crohn’s disease medications that act by blocking work of the immune system are linked with increased risk of infection, as well as a small likelihood of developing certain cancers like skin cancers and lymphoma.
- Corticosteroids may be linked with a risk of glaucoma, osteoporosis, bone fractures, cataracts, high blood pressure, and diabetes (1).
Diagnosis
Firstly, your doctor will likely rule out other possible causes for your symptoms, and then uses a combination of tests to help confirm a diagnosis of Crohn’s disease, including:
- Lab tests
- Blood tests
- Stool studies
- Procedures
- Colonoscopy
- Computerized tomography (CT)
- Magnetic resonance imaging (MRI)
- Capsule endoscopy
- Balloon-assisted enteroscopy (1).

Crohn’s Disease Treatment – Conventional Medicine, Herbal remedies, Crohn’s Disease Diet and Supplements for Crohn’s Disease
Conventional Medicine
Currently, there is no cure for Crohn’s disease. Also, there is no one treatment that is effective for everyone. The main goals of treatment are lessening the inflammation which triggers the signs and symptoms, and improving long-term prognosis by limiting complications. In the best cases, this may lead not only to symptom relief but also to long-term remission (1).
Anti-inflammatory drugs. These medications are frequently the first step in the treatment of IBD (inflammatory bowel disease). Anti-inflammatory drugs include:
- Corticosteroids. Corticosteroids can help lessen inflammation in your body. However, these medicines don’t work for all people with Crohn’s disease. Doctors may use corticosteroids only if you don’t respond to other treatments, or also in combination with an immune system suppressors.
- Oral 5-aminosalicylates. These drugs have been widely used in the past but now are generally considered of very limited benefit (1).
Immune system suppressors. These drugs also lessen inflammation, but by targeting your immune system, which produces the substances that cause inflammation. For some patients, a combination of these medications may work better than one drug alone. However these medications may have side effects, so you will need to be followed closely for side effects. Immune system suppressors include:
- Azathioprine. Side effects include lowered resistance to infection and inflammation of the liver, nausea and vomiting.
- Methotrexate (1).
Biologics. Biologics, which target proteins made by the immune system, and are used to treat Crohn’s disease include:
- Natalizumab and vedolizumab.
- Infliximab, adalimumab and certolizumab pegol.
- Ustekinumab (1).
Antibiotics. These may lessen the amount of drainage from fistulas and abscesses and sometimes heal them in people with Crohn’s disease. According to some researchers antibiotics may also help reduce bad intestinal bacteria that may play a role in triggering the intestinal immune system, and cause inflammation. Antibiotics prescribed for Crohn’s may include:
- Ciprofloxacin
- Metronidazole (1).
Other medications. Certain other medications may also help control inflammation, and relieve your signs and symptoms. However, always consult your doctor before taking any over-the-counter drugs. Other medications include:
- Anti-diarrheals. For example fiber supplements, such as psyllium powder or methylcellulose, may help alleviate mild to moderate diarrhea by adding bulk to your stool. For more severe diarrhea, loperamide may be effective.
- Pain relievers.
Vitamins and supplements. If your body does not absorb enough nutrients, and you are suffering from nutrient deficiency, your doctor may suggest vitamins and nutritional supplements (1). See the list of most often recommended nutrients and vitamins in Crohn’s disease below.
Nutrition therapy. To allow the bowel to rest (in the short term, bowel rest may also lessen inflammation), and to improve your overall nutrition, your doctor may suggest:
- Enteral nutrition. A special diet given by mouth or a feeding tube
- Parenteral nutrition. Nutrients infused into a vein.
- A low-fiber or low residue diet to lessen the likelihood of intestinal blockage if you have a narrowed bowel (stricture). A low residue diet is designed to reduce the size and number of your stools (1).
Surgery. If drug therapy, lifestyle changes, diet or other treatments don’t relieve your symptoms, your doctor may suggest surgery. However, the benefits of surgery for Crohn’s disease are usually temporary, and surgery does not cure Crohn’s disease (1).
Herbal Remedies and Supplements for Crohn’s Disease
For individuals with Crohn’s disease, the goal is to achieve and maintain remission as long as possible. While there are several prescription medications that can help you manage and relieve the symptoms, some people prefer to try alternative medicine.
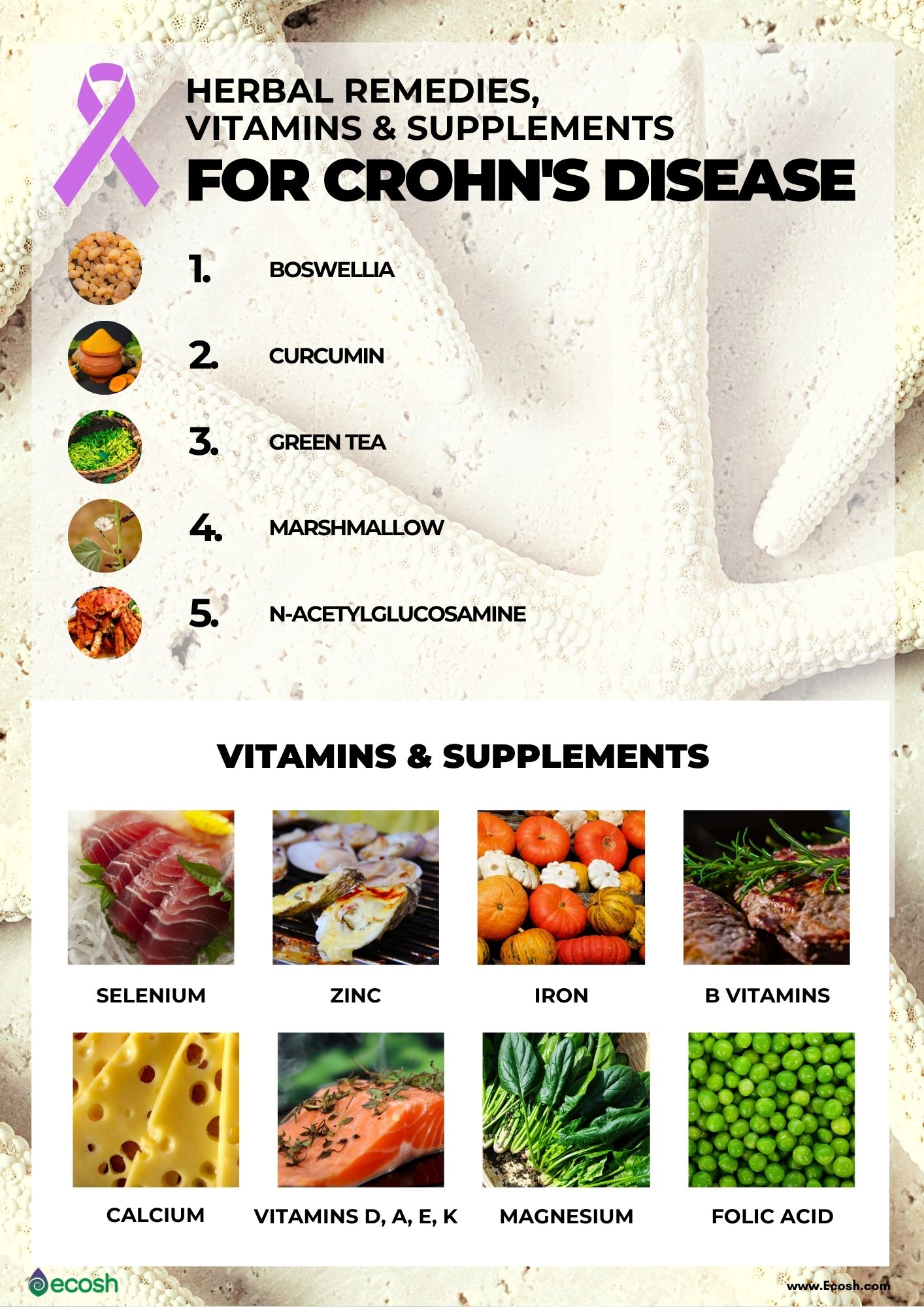
Herbal Remedies for Crohn’s Disease
Boswellia. It’s believed that Boswellia serrata may act as an anti-inflammatory agent. According to a study, 14 out of 20 people with Crohn’s disease who took boswellia supplements achieved remission. Boswellia is sometimes used also for the treatment of inflammation, asthma, and depression. Boswellia supplements are derived from trees that produce a sweet-smelling resin (acid in the resin is the active ingredient) rich in carbohydrates, essential oils, and boswellic acids (5, 6).
Curcumin in Turmeric. Extensive studies in the last two decades suggested that curcumin, the active compound in turmeric possesses anti-inflammatory, anticancer, antiviral, anti-amyloid, antiarthritic and antioxidant properties. This may help fight infections in people with Crohn’s. However, one major challenge in using turmeric to treat Crohn’s is delivering a high enough dose. This is because people with Crohn’s have trouble absorbing turmeric during digestion. Currently, researchers are developing different ways to deliver turmeric into the body for maximum absorption. Additionally, the health risks of consuming turmeric must be considered for each person. The compound may worsen gallbladder illnesses, interact with blood-thinning medications and interfere with iron absorption. When curcumin is in the body, it may also act similarly to hormones. You should speak to your doctor before taking this supplement if you have a condition that’s sensitive to hormones (6, 16).
Green Tea. Green tea polyphenols are involved in inflammatory processes and seriousness of symptoms that burden inflammatory bowel disease (IBD) patients. According to an animal study, green tea polyphenols might possess anti-inflammatory properties and lessen colon inflammation. However, it might not have the exact same effects on people, but there are no risks in consuming it (5, 7, 15).
Marshmallow. According to research, a herb called marshmallow (comes from the Althaea officinalis plant) may soothe tissues during healing, particularly in the stomach which may also lessen inflammation in people with Crohn’s. In addition, the root guards the lining of the stomach, and might thereby reduce stomach acids with no apparent side effects on the body (5, 8).
N-Acetylglucosamine (also known as N–acetyl glucosamine). In some tests, N-acetylglucosamine supplements (most often derived from the outer shell of crustaceans) have been associated to be effective in treating autoimmune disorders, as the supplement may stop cells that produce inflammation. Although further studies are needed to confirm these results, according to one study N-acetylglucosamine supplements lessened colon inflammation in children with Crohn’s disease with no negative side effects (5, 9).

Supplements and Nutrients for Crohn’s Disease
One common problem among Crohn’s patients is deficiency of certain nutrients. There might be several reasons for this. Firstly, your gut is inflamed or damaged, so it’s hard to absorb vitamins, minerals, carbohydrates, fats, and water. The same problem can also be caused by surgery for Crohn’s if too much of your small intestine is removed. Secondly, you might not want to eat due to anxiety, changes in taste, pain, and diarrhea.
Diarrhea on the other hand may reduce your body’s ability to absorb carbohydrates, protein, fat, as well as water, vitamins, and minerals. Thirdly, some prescription medications for Crohn’s drugs make it harder to absorb nutrients.
In addition, the damage to your intestines may lead to blood loss over time. This in turn could lower your iron levels and cause anemia. Therefore, with Crohn’s disease, you’re more likely to have lower levels of nutrients such as vitamin D, vitamin B-12, vitamin B6, and vitamin B1, iron, vitamin K, folic acid, selenium, and zinc.
The big question is, what is the best way to get and absorb sufficient amounts of these nutrients if you have Crohn’s disease? Although, in normal circumstances almost any diet expert suggests getting vitamins and minerals from foods, in Crohn’s disease, supplements may help fill the gaps.
Especially because Crohn’s patients may need more calories and nutrients than other people. However, always consult your doctor before starting to take any dietary supplements, as while they can help you be better nourished, some can affect the way your Crohn’s medications work or make your symptoms worse.

Crohn’s patients commonly have lower levels of nutrients such as:
Vitamin D. Vitamin D is necessary for maintaining normal levels of calcium and phosphorus in the blood, which strengthen bones and prevents osteoporosis. However, according to research, people with Crohn’s disease have lower vitamin D concentrations compared with healthy people, and over 50% of them have hypovitaminosis D. Even more, there might be an inverse correlation between circulating vitamin D concentrations and severity of Crohn’s disease. Therefore, adding vitamin D into the diet may help reduce symptoms and increase immune system health in people with Crohn’s (5, 13, 14, 17).
Vitamin B-12. This vitamin is necessary for producing new cells, protecting nerve cells, helping to make red blood cells, breaking down proteins and fats in the body. However, people with Crohn’s often suffer not only from vitamin B-12 deficiency, but also B-6, and B-1 deficiency (5, 11, 12, 13, 17).
Iron. Iron deficiency (anemia) is a frequent complication for Crohn’s disease patients. However, as for Crohn’s disease patients oral iron absorption is very limited, intravenous iron therapy has been usually recommended (10, 13, 17).
Folic Acid. Certain Crohn’s medications, such as methotrexate and sulfasalazine, lower your body’s levels of folic acid. Therefore, your doctor may suggest you to take a folate supplement (13, 17).
Calcium. Intestinal inflammatory processes reduce the absorption of sodium, chloride and calcium, while they increase potassium secretion. Also, some Crohn’s disease drugs (steroids) may weaken your bones. Moreover, if you cannot digest milk or milk products, you’re at even higher risk to develop calcium deficiency. Therefore, your doctor may recommend you to take calcium supplements to keep your bones healthy and prevent other problems like osteoporosis. However, for strong bones, and in order to absorb calcium, you also need vitamin D (13, 17, 19).
Vitamins A, E, and K. If you had surgery on your intestines, it can make it hard for your body to absorb fats, which also lowers your levels of vitamins A, E and K. So you might need to take supplements or eat foods rich in these vitamins (13, 17).
Zinc. Inflammatory bowel disease (IBD) patients with serum zinc deficiency are more likely to have adverse disease-specific outcomes. Your doctor may suggest a daily supplement to raise your levels (13, 17, 20).
Magnesium. Magnesium is an essential trace mineral, which plays a key role as an immunomodulator in many pathways leading to homeostasis. Hypomagnesemia (disturbance caused when there is a low level of serum magnesium (less than 1.46 mg/dL)) is common in patients with Crohn’s disease and may be the cause of upregulation of pro-inflammatory factors leading to aggravating symptoms. Therefore, understanding the role of magnesium in maintaining a healthy immune response is important for effective treatment of patients with CD (13, 18, 22).
Selenium. In studies, people with Crohn’s disease have been reported to be selenium deficient compared with controls. In particular, patients who have undergone bowel resection surgery have a decreased ability to absorb nutrients, including selenium (13, 17, 21).

Crohn’s Disease Diet
Although Crohn’s disease may not be the consequence of bad reactions to certain foods, paying extra attention to your diet may help replace lost nutrients, lessen symptoms, and elevate healing. In addition, some soft, bland foods may cause less discomfort during flare ups than spicy foods, high-fiber foods, or or dairy (if you are found to be lactose-intolerant). However, consult with your dietitian or doctor before making any changes to your diet (23).
Meal Planning and Food Preparation Tips
Although there is no one suggestion that suits for all Crohn’s patients, these tips may help lead you toward healthier daily nutrition:
- Consider eating 4 to 6 smaller meals daily.
- Drink enough. If your body is hydrated enough your urine should be light yellow to clear. Drink water, rehydration solution, broth, or tomato juice.
- Drink slowly and do not use a straw, as you may ingest air, which can cause gas.
- Keep your kitchen stocked with foods that you tolerate well (see list below).
- Introduce new foods slowly.
- Prepare meals in advance.
- Use healthy and simple cooking methods such as boiling, grilling, poaching or steaming.
- You can use a food journal that helps you keep track of what you eat and any symptoms that might occur due to food that you might not tolerate well (23).

Crohn’s Disease Diet – Eating When You are in a Flare
Certain foods may trigger bloating, cramping, and/or diarrhea, so you may want to avoid when you are in a flare. You should avoid trigger foods also if you have had a recent surgery, or have been diagnosed with a stricture, a narrowing of the intestine caused by inflammation or scar tissue.
Some other foods on the other hand can be easier to digest and these may provide you with the right amount of nutrients, vitamins, and minerals without making your symptoms worse. However consult your doctor or dietitian before starting any elimination diet.
Potential trigger foods for Crohn’s patients and IBD patients include:
- Spicy foods and hot spices.
- Alcohol and caffeinated drinks. Soda, coffee and all beverages containing alcohol such as beer, wine, liquor, whiskey, and vodka.
- Lactose. Dairy products that contain lactose, such as milk, cream cheese, and soft cheeses.
- Insoluble fiber foods. Raw green vegetables (particularly cruciferous vegetables like cauliflower, broccoli, or everything with a peel), whole nuts, whole grains, and fruits with skin and seeds. These foods are hard to digest.
- Non-absorbable sugars. Mannitol, sorbitol, and other sugar alcohols found in candy, sugar-free gum, ice cream, and some types of fruits and juices like peach, pear, and prune.
- Sweet and sugary foods and drinks. Juices, candy, and pastries.
- High fat foods. Margarine, butter, coconut, cream, and other greasy, fatty, and fried food (23).
Foods Crohn’s patients and IBD patients may tolerate include:
- Lean protein. Fish, lean meats such as lean cuts of pork, and white meat poultry, eggs, soy, and firm tofu
- Low-fiber fruits. Honeydew melon, bananas, cantaloupe, and cooked fruits. These are usually suggested for individuals who have had a recent surgery or have strictures.
- Refined grains. Potato, gluten-free bread, sourdough, white pasta, white rice, and oatmeal.
- Non-cruciferous vegetables. Asparagus tips, cucumbers, squash, and potatoes. These should be consumed fully cooked, skinless and seedless.
- Homemade protein shakes or oral nutritional supplements. See the list of recommended supplements above and consult your dietitian or doctor about what supplements may fit your nutritional needs (23).

Crohn’s Disease Diet – Eating When You are in Remission
It’s vital to maintain a nutrient-rich and diverse diet, as well as being hydrated even when your symptoms have subsided, or even disappeared (remission).
Foods that can help you stay healthy and hydrated:
- Protein. Fish, lean meats such as lean cuts of pork, and white meat poultry, eggs, soy, tofu and nuts.
- Fiber-rich foods. Barley, oat bran, beans, nuts, and whole grains. However, you should avoid these foods if you have an ostomy, intestinal narrowing, or if your doctor recommends you to continue a low-fiber diet because of strictures, or recent surgery.
- Fruits and vegetables. It’s advisable to remove the peel and seeds if they bother you and eat as many different colors as you can.
- Calcium-rich foods. Green leafy vegetables (like for example spinach, kale, turnips), canned salmon or sardines with bones, dried fruit, tofu, yoghurt, cheese, and milk. However, if you are lactose intolerant, use a lactase digestive enzyme or pick lactose-free dairy products.
- Probiotic foods. Kimchi, tempeh, yogurt, kefir, miso, sauerkraut, and other fermented foods (23).
NB! The information provided here is for informational purposes only, so do not consider it as health care or medical diagnosis and treatment. Do not consider this information as a guarantee of the results you want to achieve. In addition, this information here is not intended to replace the advice of your physician or other healthcare professional.
Even more, you should not use it to diagnose or treat a health problem. Before changing or discontinuing your existing medication, treatment, or care, or taking any dietary supplements, be sure to consult with your healthcare professional or doctor before starting any diet or program, or if you suspect you may have a medical condition.
Compiled by Maria-Helena Loik
Pictures: Pexels.com, Pixabay.com, Shutterstock.com
Sources:
- Crohn’s disease – Diagnosis and treatment – Mayo Clinic
- Signs and Symptoms of Crohn’s Disease | Crohn’s & Colitis Foundation
- Crohn disease: MedlinePlus Genetics
- Smoking and Crohn’s or Colitis | Crohn’s & Colitis UK (crohnsandcolitis.org.uk)
- 9 Herbs & Supplements for Crohn’s: Boswellia, Cat’s Claw, & More (healthline.com)
- Herbal and plant therapy in patients with inflammatory bowel disease (nih.gov)
- Green Tea Polyphenols and Sulfasalazine have Parallel Anti-Inflammatory Properties in Colitis Models – PubMed (nih.gov)
- Full article: Pharmacological evaluation of aqueous extract of Althaea officinalis flower grown in Lebanon (tandfonline.com)
- A pilot study of N-acetyl glucosamine, a nutritional substrate for glycosaminoglycan synthesis, in paediatric chronic inflammatory bowel disease – PubMed (nih.gov)
- TREATMENT OF ANEMIA AND IMPROVEMENT OF QUALITY OF LIFE AMONG PATIENTS WITH CROHN’S DISEASE: experience using ferric carboxymaltose – PubMed (nih.gov)
- Prevalence and Risk Factors for Functional Vitamin B12 Deficiency in Patients with Crohn’s Disease – PubMed (nih.gov)
- Vitamin B12 deficiency and IBD | IBDrelief
- Vitamins for Crohn’s Disease: Supplement Information (webmd.com)
- Vitamin D status in relation to Crohn’s disease: Meta-analysis of observational studies – PubMed (nih.gov)
- Green tea: A possibility in the therapeutic approach of inflammatory bowel diseases?: Green tea and inflammatory bowel diseases – ScienceDirect
- Curcumin: a boon to colonic diseases – PubMed (nih.gov)
- Micronutrient deficiencies in inflammatory bowel disease – PubMed (nih.gov)
- Domino effect of hypomagnesemia on the innate immunity of Crohn’s disease patients (nih.gov)
- Electrolyte and acid-base disorders in inflammatory bowel disease (nih.gov)
- Zinc Deficiency is Associated with Poor Clinical Outcomes in Patients with Inflammatory Bowel Disease (nih.gov)
- Selenium and inflammatory bowel disease (nih.gov)
- Hypomagnesemia – StatPearls – NCBI Bookshelf (nih.gov)
- What Should I Eat? | Crohn’s & Colitis Foundation