Menopause is a totally natural biological process, the phase of your life when your menstrual cycle ends, and as it is simply a matter of time when it happens. In general, menopause occurs when women are in their 40s or 50s (the average age is 51), and is determined after 12 months without a menstrual period.
The symptoms of menopause can sometimes be severe, and seriously disrupt daily life, like for example disturb sleep, lower energy or influence emotional health.
Treatment options include hormone therapy, certain medications, lifestyle changes, alternative medicine, herbal remedies, nutritional supplements and diet.
Though, there is no warranty that following a certain lifestyle, or taking some herbal remedies or supplements will relieve the symptoms of menopause, there are still various things you can try (20).
Menopause and Perimenopause Signs and Symptoms
Signs and symptoms can be different among women. Some women face only trivial symptoms while others undergo severe symptoms. However, during perimenopause (the time before menopause when women gradually produce less estrogen), the most common sign among all women is irregularity in menstrual periods.
Menstrual periods may occur on shorter cycles, or skip a month and then start again, or skip several months and then return for a few months. Perimenopause can last months or sometimes even years.
Although your menstrual cycle is irregular, you can still get pregnant.
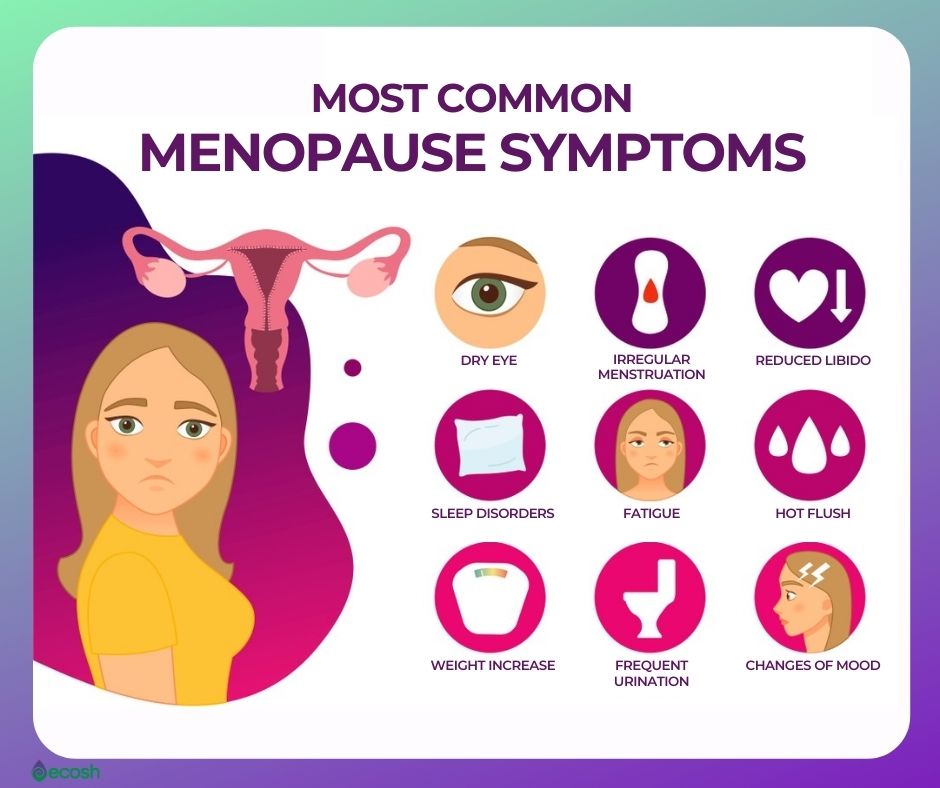
The signs and symptoms include:
- Irregular periods, less frequent menstruation
- Heavier or lighter periods than usually
- Vaginal dryness
- Night sweats
- Flushing
- Hot flashes (about 75 % of women experience hot flashes during menopause)
- Chills
- Sleep problems and insomnia
- Mood swings
- Slowed metabolism and weight gain
- Dry skin, eyes and mouth
- Thinning hair
- Changes in libido (for example reduced sex drive)
- Memory problems and difficulty concentrating
- Depression
- Anxiety
- Increased urination
- Increased hair growth for example in the face, neck, chest, and upper back
- Headaches
- Racing heart
- Urinary tract infections (UTIs)
- Decreased muscle mass
- Painful or stiff joints
- Reduced bone mass
- Tender or sore breasts
- Loss of breast fullness (2, 4, 5).
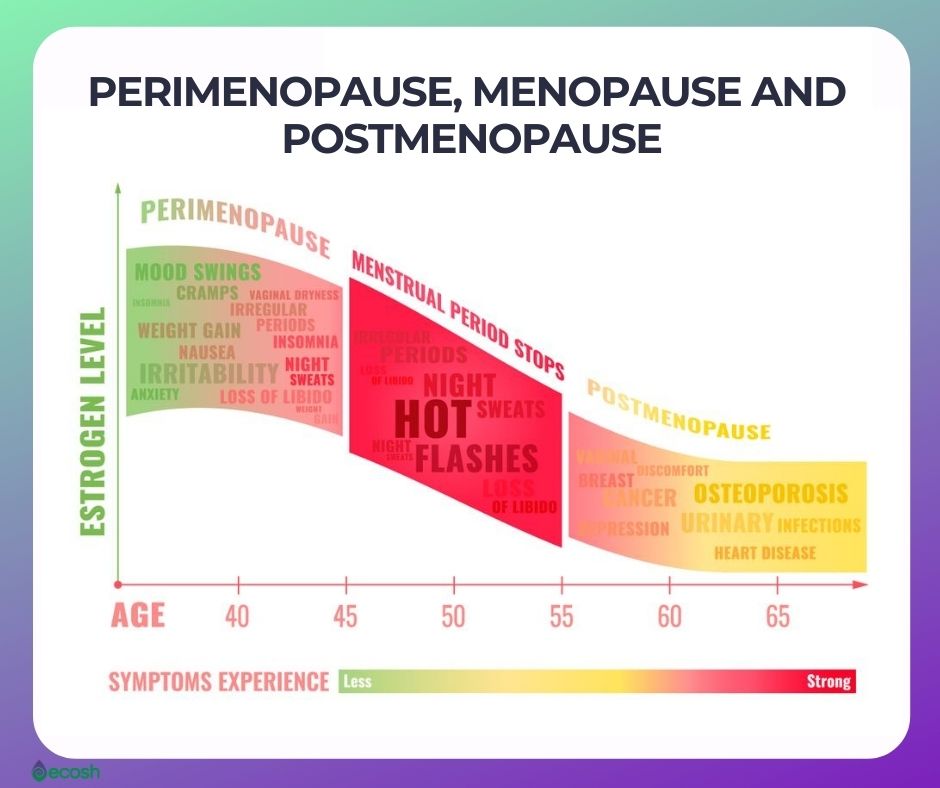
Difference Between Perimenopause, Menopause and Postmenopause
- Perimenopause. Your menstrual cycle (periods) becomes irregular, or you may completely skip periods one or several times.
- Menopause. Missing menstrual cycle for one year.
- Postmenopause. The time after menopause has happened (5).
Natural Menopause and Premature Menopause (Early Menopause) Causes
Menopause can be natural or induced:
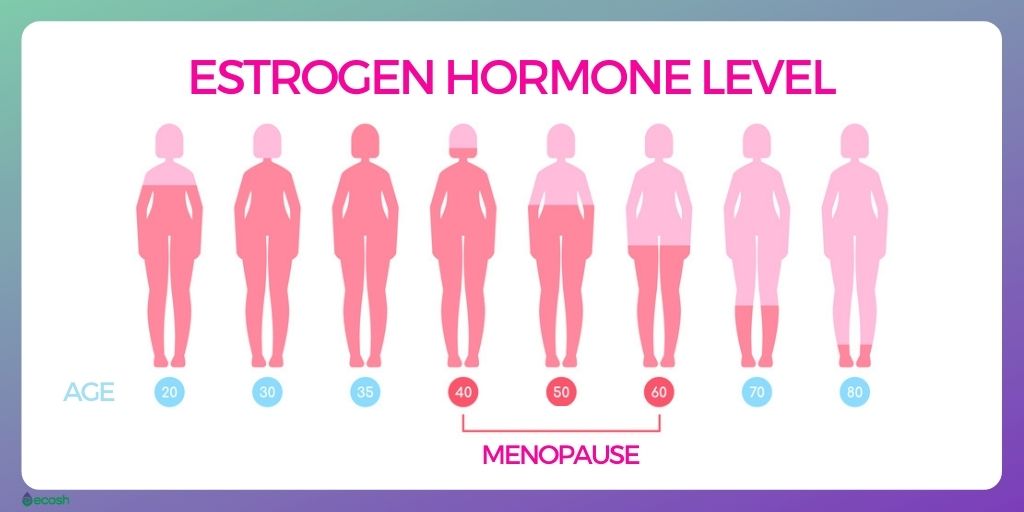
Age – naturally decreasing reproductive hormones. Due to aging ovaries, and lower levels of hormones estrogen, progesterone, testosterone, follicle-stimulating hormone (FSH), and luteinizing hormone (LH) – your body begins to undergo several changes. One of the most notable changes is the loss of active ovarian follicles (the structures that produce and release eggs from the ovary wall).
- Late 30s. Your ovaries start producing less hormones (estrogen and progesterone) already in your late 30s, so this is the time when these changes are slowly starting.
- Mid-to-late 40s. At some point during this time your menstrual periods may become longer or shorter, heavier or lighter, and more or less frequent.
- 50s. Your ovaries do not release eggs anymore, and most women have undergone menopause by the age 51.
Ovarian ablation, or the shutdown of ovary function. In addition to surgery, and radiotherapy techniques, this may be done also by hormone therapy in women with estrogen receptor-positive tumors.
Bilateral oophorectomy or surgery that removes the ovaries (oophorectomy). As hormones that regulate menstrual cycle are produced by ovaries – surgery which removes your ovaries leads to immediate menopause. In this case, periods stop instantly and symptoms of menopause can be severe, because hormonal changes happen all at once rather than gradually over several years.
Pelvic injuries.
Chemotherapy and radiation therapy. These treatments can lead to symptoms such as hot flashes during or shortly after the treatment, and prompt menopause. After chemotherapy, the pause in menstruation (and fertility) is not always permanent, therefore, you may still need birth control measures. Radiation therapy does not affect ovaries if it’s done to other parts of the body.
Primary ovarian insufficiency. About 1 % of women undergo menopause uncommonly early (premature menopause), which means menopause starts before age 40. This may be the consequence of the failure of ovaries to produce normal levels of reproductive hormones (primary ovarian insufficiency). In order to protect the bones, brain, and heart, hormone therapy is usually suggested (at least until the natural age of menopause) for women with this condition.
Smoking. According to a study, cigarette smoking has been found to speed up the onset of menopause by as much as one year (4, 5, 6).
Premature Menopause (Early Menopause) Risk Factors
Premature menopause (also early menopause or premature ovarian failure) happens when a woman begins menopause before age 40. Risk factors include:
- Autoimmune diseases (such as for example rheumatoid arthritis)
- Epilepsy
- Chromosome defects
- Thyroid disease
- Smoking
- Medications that reduce estrogen
- Surgeries
- Chemotherapy and radiation
- Vegetarian diet (6, 7, 9).
Premature Menopause (Early Menopause) Prevention
Although some cases of premature menopause are unavoidable, there are also some cases where it might be possible to prevent or delay it if to take some steps:
- Stop smoking
- Maintain a healthy weight
- Exercise regularly
- Use natural skin care products to avoid hormones or substances that may act like hormones in other skin care products.
- Avoid processed foods, as according to a study – refined carbohydrate sources in the diet seem to hasten menopause.
- Eat natural, healthy foods as much as possible (especially those rich in phytoestrogen, antioxidants and omega-3 such as oily fish, beans and other legumes). According to a study, consuming a portion of oily fish, beans, and other legumes every day may be linked with an average 3.3-year delay in the start of menopause. While on the other hand extra portions of rice or refined pasta every day, is associated with about 1.5 years earlier menopause. It’s not clear why it is like that, but researchers speculated that the antioxidants in legumes and the omega-3 fatty acids in certain fish might have a protective influence on your eggs, basically helping to protect them for longer and setting back the start of menopause.
- Vitamin B6 and zinc. Higher consumption of zinc (about 0.3 years delay) and vitamin B6 (about 0.6 years delay), also seem to delay menopause.
- In addition, vegetarians in one study reached menopause at an earlier age than meat eaters (6, 7, 8, 9, 10, 11).
Menopause Complications
As estrogen levels in your body decrease, the likelihood of developing certain conditions increases.
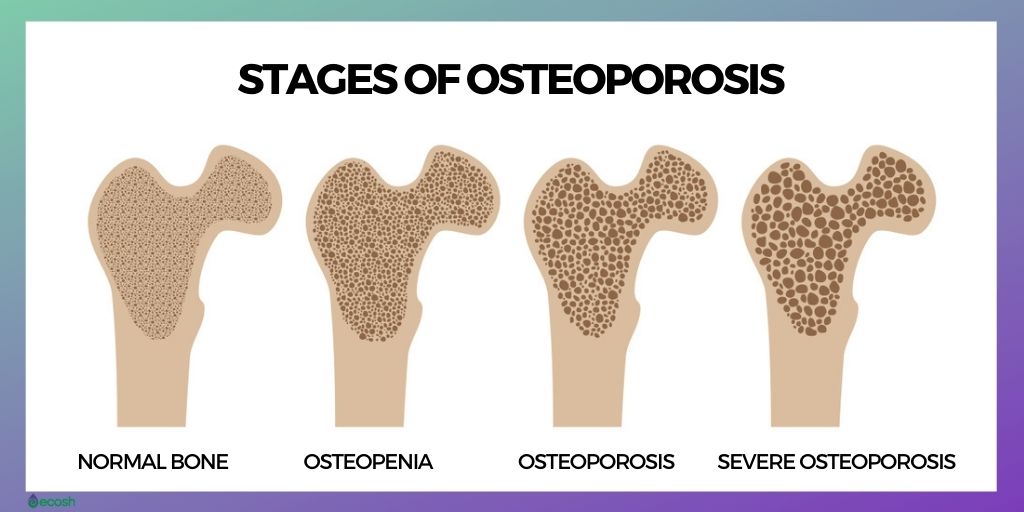
Osteoporosis. In case osteoporosis, bones lose their density and become brittle, leading to an increased risk of fractures. In the course of the first few years after menopause, you may lose bone density at a high-speed rate. However, healthy weight, exercise, and sufficient amounts of certain nutrients such as vitamin D, calcium, and magnesium may help to prevent this condition.
Cardiovascular (heart and blood vessel) disease. The risk of cardiovascular disease increases when estrogen levels decrease. However, maintaining a healthy weight, exercising regularly, eating a healthy diet and keeping your cholesterol levels and blood pressure under control, may lessen the risk.
Atrophic vaginitis or vaginal atrophy. The thinning of the walls of the vagina which is caused by reduced estrogen levels.
Urinary incontinence. As you get older, the elasticity of your urethra and vagina decreases which may lead to intense, frequent and sudden urges to urinate, followed by an unwilling loss of urine (urge incontinence). Involuntary loss of urine may also happen due to laughing, lifting, sneezing, running or coughing (stress incontinence). In addition, you may experience urinary tract infections more often.
Decreased sexual function and libido. Sexual intercourse may cause discomfort and sometimes also slight bleeding, because of the decreased moisture production (which leads to vaginal dryness), lowered sensation, and reduced elasticity. Due to all these changes you might not have as much desire for sexual activity as before.
Dyspareunia (painful intercourse). Sharp or intense recurring pain within the pelvis or in the genital during sexual intercourse. Dyspareunia can occur before, during, or after sexual intercourse.
Slower metabolic function and weight gain. Gaining weight during the menopausal transition, and after menopause is very common, because your metabolism slows. Therefore, just to maintain your current weight – you may need to exercise more and eat less.
Mood swings or sudden emotional changes. When estrogen levels change during menopause, your mood may change with it, as estrogen helps to support certain types of brain functions (such as cognition). This decrease in estrogen can also cause Some women may sometimes experience episodes of forgetfulness, or “fuzzy-brain”.
- Periodontal disease. Hormonal changes in women may lead to periodontitis which is a severe infection of the gums (4, 5).
Menopause Treatment – Conventional Medicine, Vitamins, Herbal Remedies, Alternative Medicine and Home Treatment
Conventional Medicine
Menopause does not need medical treatment. Therefore, treatments usually focus on relieving your signs and symptoms and preventing or managing chronic conditions that may occur with aging and menopause. Before making any decisions, consult with your doctor about your possibilities and the risks and benefits involved with each treatment. Treatments may include:
- Hormone therapy
- Vaginal estrogen
- Low-dose antidepressants
- Gabapentin (Gralise, Horizant, Neurontin)
- Clonidine (Catapres, Kapvay)
- Medications to prevent or treat osteoporosis or vitamin D supplements to help strengthen bones.
5 Vitamins That May Help Minimize The Symptoms of Low Estrogen and Menopause
According to studies, a balanced supply of the selected vitamins might contribute to improving the quality of life in menopausal women. However, consult your doctor before taking any new supplement and use all listed vitamins with caution, as in some cases some vitamins might have unwanted side effects or they might interact with your current medications or health conditions (2, 3).
Vitamin D:
- Bone health and preventing osteoporosis. Vitamin D is vital for bone health, and it may help prevent osteomalacia (softening of the bones) and osteoporosis (reduced bone density) which is especially important throughout menopause, as hormonal changes during this time contribute to osteoporosis. Some women may lose up to one-fifth of their bone density in the 5–7 years after menopause. However, getting enough vitamin D and calcium around menopause can help prevent this (2, 3, 13, 16).
- Recommended intake up to the age of 70: 600 IU (international unit)
- Recommended intake from 71 onward: 800 IU (international unit) (18).
- You can read more about the 16 health benefits of vitamin D here.
Vitamin C:
- Hot flashes, and insomnia. Several studies have shown the benefits of vitamin C combined with citrus bioflavonoids for relieving hot flashes, and insomnia.
- Cognitive function and bone density. Vitamin C supplementation might also be correlated with a significant improvement in cognitive function and higher bone density among menopausal women.
- Antioxidant benefits. Even more, as vitamin C is a strong antioxidant, it may also help to lessen the risk of some conditions that can result from oxidative stress, such as some types of cardiovascular disease.
- Immune system and collagen production. Vitamin C also plays a critical role in the immune system as well as in the production of collagen (3, 12, 13).
- You can read more about the 12 health benefits of vitamin C here.
B Group Vitamins:
- Cardiovascular disease, stroke, and dementia. Sufficient amounts of B vitamins may help prevent cardiovascular disease, stroke, and dementia, all of which can begin during menopause and are a risk for older people.
- Nervous system. B vitamins play a vital role in maintaining the functions of the nervous system.
- Bone density. Individuals with low levels of vitamin B-2, B-6, and B-12 may also have reduced bone mineral density, a factor for osteoporosis.
- Cognitive function. Vitamins B-6 and B-12 may help support cognitive function and high intake on vitamin B-6 may lower the risk of depression in all older people, including those undergoing menopause.
- Serotonin levels, depression and loss of energy. Taking a vitamin B-6 supplement during and after menopause may help tame prevent symptoms caused by low serotonin levels (including loss of energy and depression).
- Hot flashes. Moreover, according to study, vitamin B-9, (folate), might also be effective in reducing the severity and number of hot flashes (2, 3, 13, 14, 15).
- Vitamin B-12 recommended dietary allowance (RDA) for females 14 and older: 2.4 micrograms (mcg) daily.
- Vitamin B-6 recommended dietary allowance (RDA) for females 19 and older: 100 milligrams (mg) daily.
- You can read more about the health benefits of vitamin B-6, and vitamin b-12, and B-group vitamins overall.
- To meet these recommended daily allowances you can eat vitamin B rich foods or take vitamin B-12, vitamin B6, or B complex supplements.
Vitamin E:
- Antioxidant benefits. Like vitamin C, vitamin E is also an antioxidant, necessary in fighting against free radicals that cause oxidative stress which in turn may cause several other health conditions.
- Stress, anxiety and depression. Scientists also associate low levels of antioxidants with anxiety and depression, which many women experience during menopause. Therefore, vitamin E may help ease stress, reduce oxidative stress, and help reduce your risk of depression.
- It is suggested to take at least 15 mg daily (2, 13, 17).

Herbal Remedies That May Help Minimize The Symptoms of Low Estrogen and Menopause
Although hormone therapy long was considered the first line of treatment for vasomotor symptoms such as night sweats, hot flashes, and flushes, many women are turning to botanicals and dietary supplement (BDS) products for relief (despite the fact that there is limited scientific evidence describing efficacy and long term safety of all these products. Therefore, consult your doctor before starting to consume any of these) (1).
Black cohosh. Black cohosh shows great promise in relieving menopausal symptoms such as primarily night sweats, hot flashes, flushes and possibly mood disorders with an overall positive safety profile for up to six months. However, according to MayoClinic black cohosh supplement may be unsafe for women with a history of breast cancer, and may be harmful to the liver (1, 20).
Soy/isoflavones. The data on the results of soy/isoflavones for menopausal symptoms is minimal. However, considering the cardiovascular benefits as well as the potential beneficial effects on bone and possibly cognition, it would seems that soy in the diet of peri and postmenopausal women (who do not have a soy allergy), is beneficial (1).
St. John’s wort. Has been shown to improve mild to moderate depression in the general population and seems to show efficacy for mood disorders related to the menopausal transition. May improve sexual well-being (1).
Red clover. Minimal effect in relieving menopausal symptoms, however similar to soy/isoflavones, it remains to be seen if it will have uses for age related health concerns such as osteoporosis, heart disease, and cognition (1).
Dong quai root. Hot flash incidence decreased among these women who consumed dong quai, however, compared to placebo, the effect is not significant (1).
Korean red ginseng. Red ginseng improved fatigue, insomnia and depression. Cortisol/DHEA-S ratio was significantly decreased (1).
Kava extract. Significant improvement in Kupperman index (an 11-item menopausal symptom questionnaire that has been used in hundreds of clinical studies to determine menopausal symptom prevalence and to evaluate the efficacy of an array of therapies intended to alleviate menopausal symptoms) and HAMA anxiety score (The Hamilton Anxiety Rating Scale is a psychological questionnaire used by clinicians to rate the severity of a patient’s anxiety) (1).
Vitex agnus castus oil. 33% of women reported major improvement in troublesome symptoms, most often emotional problems and hot flashes (1).
Sage. The herb sage is thought to contain compounds with estrogen-like effects, and there’s good evidence that it can effectively manage menopause symptoms. However, avoid it if you have an allergy to sage, or if you are pregnant or breast-feeding women. Also, use it carefully if you have high blood pressure or epilepsy (20).
Flaxseed. Although there is not enough scientific evidence, some believe that consuming some form of flax seeds (also called linseed) – may help to reduce hot flashes (24, 25, 26).
Licorice. Licorice is often used as part of a multi-botanical formulation and is thought to be useful for PMS, but is largely unstudied in menopause (1).
Many of the aforementioned botanicals are not used alone but rather in combination with other supplements in the form of a multi-botanical, of which there is even less science to support efficacy and safety (1, 19).
Alternative Medicine, Diet, Lifestyle and Home Remedies
Many of the symptoms linked with menopause are temporary. Here are some tips to help reduce or prevent their effects:
Hot flashes and night sweats. Triggers may include caffeine, hot beverages, alcohol, spicy foods, stress, hot weather, a warm room, smoking, wearing tight, restrictive clothing or using heavy blankets or sheets on your bed. If you know your trigger, if possible try to avoid it. Other tips include dressing in layers, and having a bottle with cold water with you (20, 24).
Vaginal discomfort. You can try all over-the-counter water-based vaginal lubricants or a silicone-based lubricant or moisturizer. However, products that contain glycerin may cause burning or irritation in case you’re sensitive to that chemical. Being sexually active may also help with vaginal discomfort, as it increases blood flow to the vagina (20).
Decreased sexual function and libido. Certain OTC moisturizers, water-based vaginal lubricants, or local vaginal estrogen treatments may help.
Urinary incontinence. Exercises that strengthen pelvic floor muscles (Kegel exercises) may help lessen these uncomfortable symptoms.
Sleeping problems. Caffeine and drinking too much alcohol may make it hard to get to sleep or can interrupt sleep. So try to avoid these beverages. Exercising during the day (not right before bedtime) may help you get better sleep. If hot flashes disturb your sleep, here are some tips:
- Calming routine before bedtime (in soft light)
- Turn down the temperature in your bedroom
- If possible, sleep with window open
- Use a bedside fan
- Remove heavy blankets or sheets
- Turn your pillow often
- Wear loose, light clothing, change into cool clothes or dress in layers so you can remove them and add them according to your body temperature
- Maintain a healthy weight
- You can use cooling gels, cooling sprays, or pillows
- Sip cool water
- Breathing exercises – slowing and deepening your breathing to help your body relax (20, 24).
Relaxation techniques. Some techniques such as for example progressive muscle relaxation, deep breathing, paced breathing, guided imagery, and massage may help relieve some menopausal symptoms (20).
Strengthening your pelvic floor. Kegel exercises (pelvic floor muscle exercises) may be effective in improving some types of urinary incontinence (20).
Smoking. Try to quit smoking, as it increases your risk of osteoporosis, heart disease, stroke, cancer and a variety of other health conditions. It may also increase hot flashes and bring on earlier menopause (20).
Exercising, yoga and tai chi. Although there is no evidence to support the practice of yoga in reducing menopausal symptoms, balance exercises such as yoga or tai chi can improve coordination as well as strength, and any regular exercise helps to protect against diabetes, heart disease, osteoporosis and several other conditions linked with aging. However, do not start to self practice and consult an expert who can guide you (20).
Acupuncture. Although more research is needed, acupuncture may have some effect in helping to reduce hot flashes (20, 22, 23).
Hypnosis. According to research, hypnotherapy may lessen the incidence of hot flashes for some menopausal women (20, 21).
Bioidentical hormones. There’s no scientific evidence that bioidentical hormones (the hormones in the product (which come from plant sources) are chemically identical to those your body produces) work any better or are any less risky than traditional hormone therapy in easing menopause symptoms (20).
Diet:
- Consult your doctor if you might need calcium or vitamin D supplements to help meet daily requirements, as these nutrients are extremely important during menopause to prevent osteopenia and osteoporosis.
- Also, watch your diet, limit saturated fats and sugars, and increase the content of vegetables and fruits as gaining weight is very common in the course of menopause.
- Plant estrogens (phytoestrogens). There are two main types of phytoestrogens – estrogens that occur naturally in certain foods – isoflavones (found in soybeans, lentils, chickpeas and other legumes) and lignans (found in flaxseed, whole grains, and some fruits and vegetables). However, the effect of these still remains to be proved, as most studies have found them ineffective. Isoflavones have some weak estrogen-like effects, so if you’ve had breast cancer, talk to your doctor before supplementing your diet with isoflavone pills (20, 24, 25, 26).
NB! The information provided here is for informational purposes only, so do not consider it as health care or medical diagnosis and treatment. Do not consider this information as a guarantee of the results you want to achieve. In addition, this information here is not intended to replace the advice of your physician or other healthcare professional.
Even more, you should not use it to diagnose or treat a health problem. Before changing or discontinuing your existing medication, treatment, or care, or taking any dietary supplements, be sure to consult with your healthcare professional or doctor before starting any diet or program, or if you suspect you may have a medical condition.
Compiled by Maria-Helena Loik
Photos: Pexels.com, Pixabay.com, Shutterstock.com
Sources:
- Botanical and Dietary Supplements for Menopausal Symptoms: What Works, What Doesn’t (nih.gov)
- Vitamins for Menopause: What Works? (healthline.com)
- Selected vitamins and quality of life in menopausal women (nih.gov)
- Menopause – Symptoms and causes – Mayo Clinic
- Menopause: Symptoms, Causes, Treatment, and More (healthline.com)
- Factors associated with early menopause – PubMed (nih.gov)
- Risk Factors of Early Menopause (healthline.com)
- These foods may delay your menopause (medicalnewstoday.com)
- Diet might delay — or hasten — the onset of menopause – Harvard Health
- Phytoestrogens: Benefits, risks, and food list (medicalnewstoday.com)
- Efficacy of phytoestrogens for menopausal symptoms: a meta-analysis and systematic review (nih.gov)
- Menopause is helped by Vitamin C with Bioflavonoids | Pacific Center for Naturopathic Medicine (doctorherdmanclinic.com)
- Menopause: Do vitamins help? (medicalnewstoday.com)
- The Effect of Folic Acid on Menopausal Hot Flashes: A Randomized Clinical Trial (nih.gov)
- Intakes of folate, vitamin B 6 and B 12 and risk of depression in community-dwelling older adults: the Quebec Longitudinal Study on Nutrition and Aging | European Journal of Clinical Nutrition (nature.com)
- Osteoporosis – NHS (www.nhs.uk)
- Novel Therapeutic Targets in Depression and Anxiety: Antioxidants as a Candidate Treatment (nih.gov)
- Osteoporosis | womenshealth.gov
- Herbal Remedies for Menopause, Menopause Information & Articles | The North American Menopause Society, NAMS
- Menopause – Diagnosis and treatment – Mayo Clinic
- Clinical Hypnosis in the Treatment of Post-Menopausal Hot Flashes: A Randomized Controlled Trial (nih.gov)
- Acupuncture in Menopause (AIM) Study: a Pragmatic, Randomized Controlled Trial (nih.gov)
- Acupuncture may reduce menopause symptoms (medicalnewstoday.com)
- Tips for Dealing with Hot Flashes and Night Sweats (healthline.com)
- Effects of flaxseed and Hypericum perforatum on hot flash, vaginal atrophy and estrogen-dependent cancers in menopausal women: a systematic review and meta-analysis (nih.gov)
- Flaxseed Shows Potential To Reduce Hot Flashes — ScienceDaily