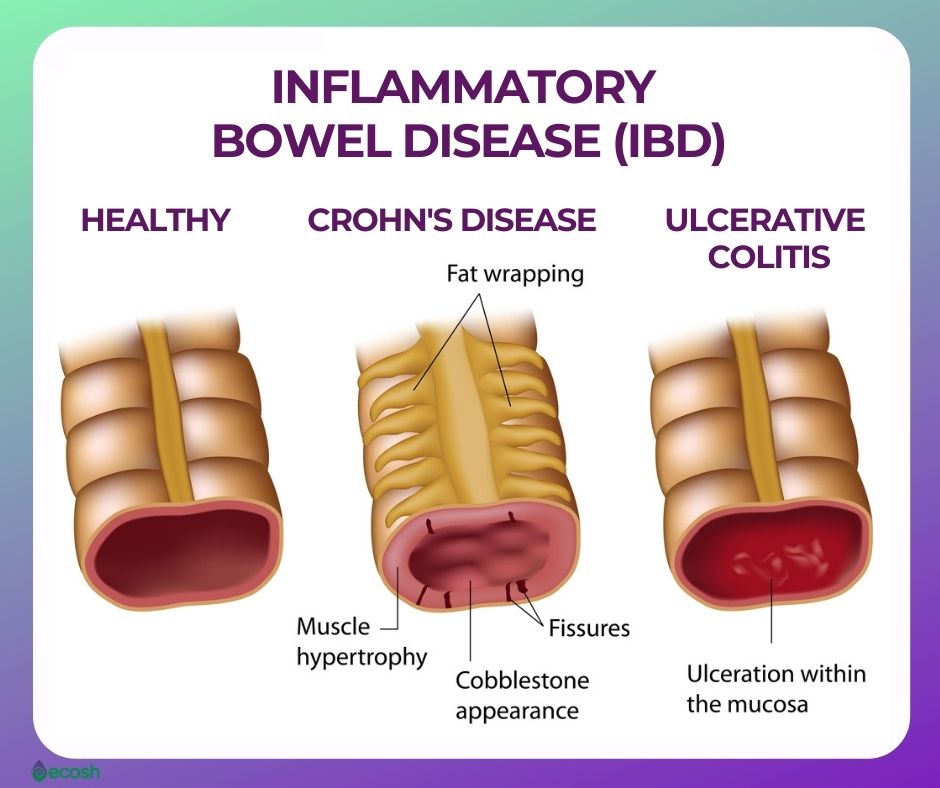
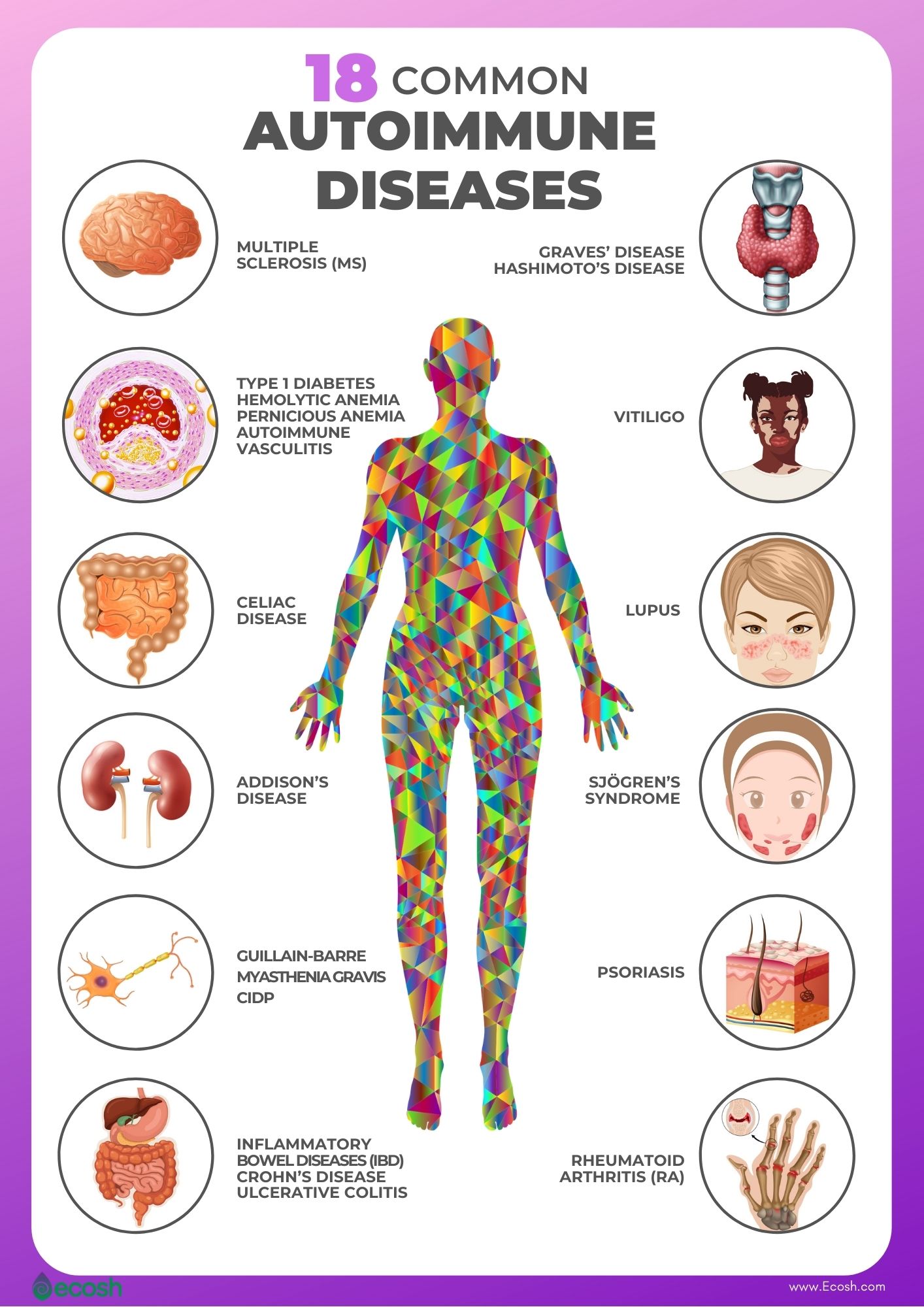
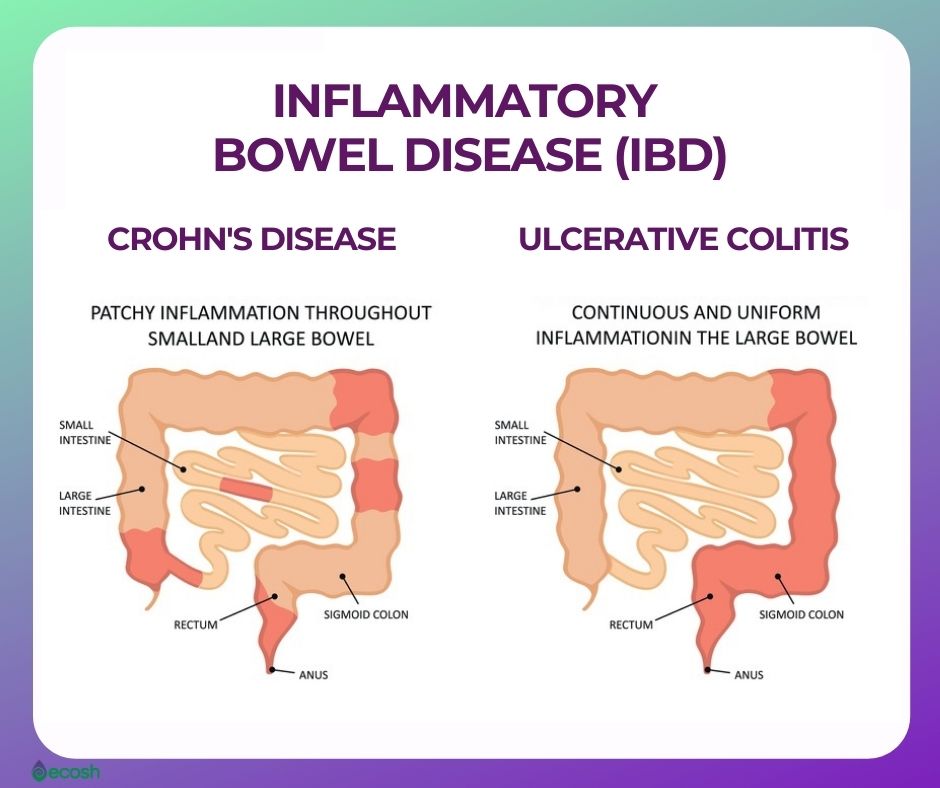
Ulcerative colitis is an autoimmune disorder, a type of inflammatory bowel disease (IBD) that causes inflammation and ulcers (sores) in your digestive tract. Inflammatory bowel disease (IBD) is an umbrella term that represents two conditions – ulcerative colitis and Crohn’s disease, that cause inflammation in the lining of the intestinal wall.
Each type of IBD affects a different part of the gastrointestinal (GI) tract.
- Crohn’s disease can affect any part of the gastrointestinal (GI) tract, from the mouth to the anus. This chronic disease causes inflammation of the digestive tract, which can involve different areas of the digestive tract in different people, and lead to malnutrition, abdominal pain, fatigue, severe diarrhea, and weight loss. Crohn’s disease can be weakening as well as painful, and it may sometimes lead to life-threatening complications.
- Ulcerative colitis. This disorder influences only the innermost lining of the large intestine (colon) and rectum. Signs and symptoms of ulcerative colitis usually develop over time, rather than suddenly.
Ulcerative colitis prevalence is 9 to 20 cases per 100,000 persons per year. Compared to Crohn disease, ulcerative colitis has a greater incidence rate in adults.
This disorder can be debilitating and can sometimes cause life-threatening complications. Although ulcerative colitis has no known cure, treatment can significantly lessen the symptoms of the disease and bring about long-term remission.
In addition, along with conventional treatment, you may find some help in supplements, alternative medicine, ulcerative colitis diet, lifestyle changes and herbal remedies (1, 11, 12).
Ulcerative Colitis Signs and Symptoms
The course and symptoms of ulcerative colitis may vary, depending on the severity of inflammation and how much of the rectum and colon is inflamed. Some ulcerative colitis patients may go for weeks or even months with extremely mild symptoms, or no symptoms at all (remission).
However, these remissions may be followed by phases where the symptoms are especially troublesome (flare-ups or relapses). Although ulcerative colitis usually isn’t fatal, it’s a serious disorder that, in some cases, may cause life-threatening complications.
Therefore, see your doctor if you experience a persistent change in your bowel habits or if you have symptoms such as blood in your stool, abdominal pain, ongoing diarrhea or diarrhea that awakens you from sleep (that doesn’t respond to OTC medications) or an unexplained fever lasting more than a day or two (1).
Common signs and symptoms of ulcerative colitis may include:
- Recurring diarrhea, often with blood, mucus or pus
- Diarrhea that awakens you from sleep
- Tummy pain and cramping
- Rectal pain
- Rectal bleeding (passing small amount of blood with stool)
- Needing to empty your bowels frequently
- Inability to defecate despite urgency
- Loss of appetite
- Weight loss
- Tiredness and fatigue
- Fever
- In children, failure to grow (1, 2).
Symptoms of a flare-up may include:
During a flare-up, and in severe cases, some individuals with ulcerative colitis may also have symptoms elsewhere in their body. For example, some people may experience:
- Areas of painful, swollen and red skin
- Swollen and painful joints (arthritis)
- Mouth ulcers
- Red and irritated eyes
- Having to empty your bowels 6 or more times a day (in severe cases)
- Shortness of breath
- A fast or irregular heartbeat
- Fever
- In addition, blood in your stools becomes more obvious (2).
Types of Ulcerative Colitis
Ulcerative colitis is often classified according to its location:
- Ulcerative proctitis. Inflammation is limited to the area closest to the anus (rectum), and typically affects less than six inches of the rectum. Ulcerative proctitis is not associated with an increased risk of cancer. The only symptom of ulcerative proctitis may be rectal bleeding, but symptoms may also include rectal pain and urgency in your bowel movements.
- Left-sided colitis. Continuous inflammation extends from the rectum up through the splenic flexure, which is a bend in the colon near the spleen. Symptoms may include loss of appetite, weight loss, bloody diarrhea, abdominal cramping, urgency to defecate, and pain on the left side of the abdomen. Left-sided colitis also includes proctosigmoiditis.
- Proctosigmoiditis. Inflammation affects the sigmoid colon (lower segment of colon located right above the rectum) and rectum. Symptoms include abdominal pain and cramps, bloody diarrhea, and an inability to move the bowels in spite of the urge to do so (tenesmus).
- Pancolitis or extensive colitis. Continual inflammation starts at the rectum and spreads beyond the splenic flexure. Therefore, this type or ulcerative colitis often affects the entire colon. Symptoms of pancolitis may include loss of appetite, fatigue, bouts of bloody diarrhea that may be severe, tummy pain, abdominal cramps, and notable weight loss (1, 3).
Ulcerative Colitis Causes
The precise triggers for flare-ups and causes of ulcerative colitis are not yet well understood. Earlier, doctors suspected that diet and stress were the culprits. However, now it`s known that these factors may aggravate ulcerative colitis, but don’t cause it.
According to some theories, several factors, such as infections, stress, heredity, genetics, environmental factors, and a malfunctioning immune system (when your immune system tries to fight off an invading virus or bacterium, an abnormal immune response causes the immune system to attack the cells in the digestive tract, too) may contribute to its development (1, 2).
Ulcerative Colitis Risk factors and Risk Groups
- Gender. Ulcerative colitis affects about the same number of women and men.
- Age. Although this condition can occur at any age, it generally begins before the age 30. However, some individuals may not develop the disease until after age 60.
- Ethnicity. Although ulcerative colitis can happen in any race, whites have the highest risk of developing the condition. Moreover, the risk is even higher in Jews of European descent (Ashkenazi). The greatest prevalence of inflammatory bowel diseases are seen in North America and Northern Europe. Therefore, it seems that inflammatory bowel diseases such as ulcerative colitis and Crohn’s disease are closely linked to a westernized environment and lifestyle.
- Heredity and genetics. As ulcerative colitis tends to run in families, you’re at higher risk of developing the disease if you have a close relative, such as a parent, sibling or child, with the disease, with the condition. The genetic factor plays a greater role with Crohn’s disease than ulcerative colitis. However, most people with ulcerative colitis don’t have a family history of the disease (1, 11).
Ulcerative Colitis Possible Complications
- Osteoporosis (bone loss)
- Severe bleeding
- Perforated colon (a hole in the colon)
- Extreme dehydration
- Inflammation of your eyes, joints and skin
- An increased risk of colon cancer
- Toxic megacolon (a rapidly swelling colon)
- In addition, increased risk of blood clots in arteries and veins (1).
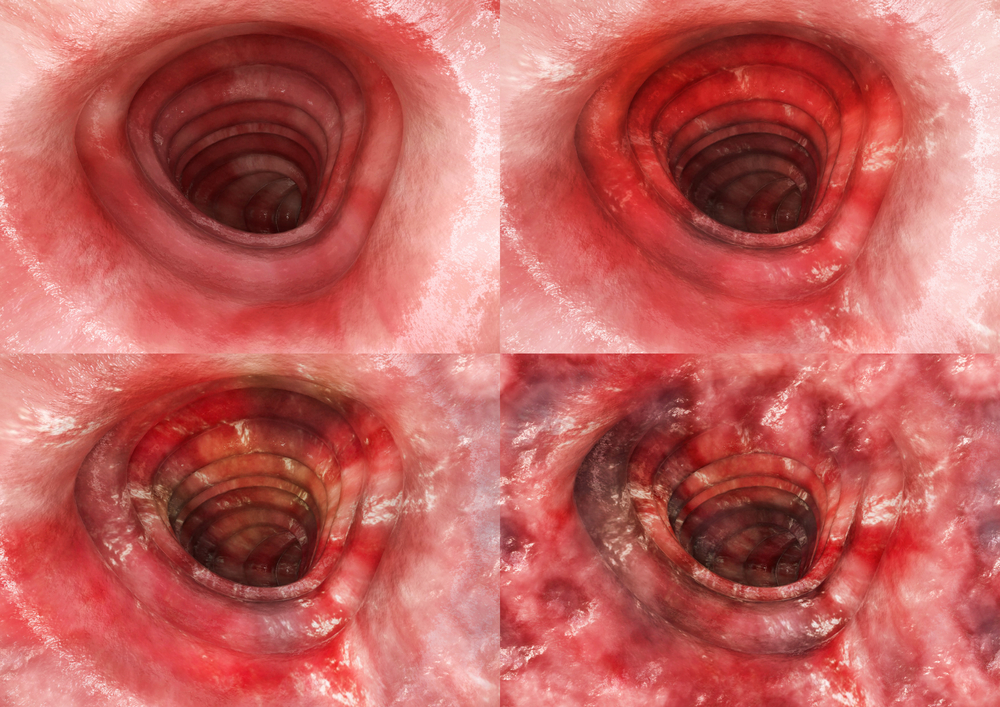
Ulcerative Colitis Diagnosis
To definitively diagnose ulcerative colitis, endoscopic procedures with tissue biopsy are the only way. Other tests can help rule out complications or other types of IBD (inflammatory bowel disease), such as Crohn’s disease. Therefore, you may have one or more of the following tests and procedures:
- Lab tests
- Blood tests
- Stool studies
- Endoscopic procedures
- Colonoscopy
- Flexible sigmoidoscopy
- Imaging procedures
- X-ray
- CT scan
- Computerized tomography (CT) enterography and magnetic resonance (MR) enterography (1).

Ulcerative Colitis Treatment – Conventional Medicine, Lifestyle Tips, Ulcerative Colitis Diet and Supplements for Ulcerative Colitis
Conventional Medicine
Ulcerative colitis treatment and the type of drug you take depends on the severity of your condition, and usually involves either drug therapy or surgery. However, it may take time to find a medicine that is helpful for you, as the drugs that work perfectly for some patients may not work for others. In addition, you’ll need to weigh the benefits and risks of any treatment, as some medications may have serious side effects.
Anti-inflammatory drugs. These medications are often the first step in the treatment of ulcerative colitis and are suitable for the majority of patients with this condition. Anti-inflammatory drugs include:
- 5-aminosalicylates
- Corticosteroids (1).
Immune system suppressors. These medications also lessen inflammation, but they do so by suppressing the immune system response that starts the process of inflammation. For some patients, a mixture of these medicines works better than one drug alone. Immune system suppressors include:
- Azathioprine and mercaptopurine
- Cyclosporine
- Tofacitinib (1).
Biologics. Biologics which target proteins made by the immune system, and are used to treat ulcerative colitis include:
- Infliximab, adalimumab and golimumab
- Vedolizumab
- Ustekinumab (1).
Other medications. In addition, certain other medications may also help control inflammation or other specific symptoms of ulcerative colitis. However, always consult your doctor before taking any over-the-counter drugs, as these may have unwanted side effects. Other medications include:
- Anti-diarrheal medications (loperamide)
- Pain relievers (acetaminophen, but not ibuprofen, naproxen sodium, and diclofenac sodium, as these can worsen symptoms and increase the severity of disease)
- Antispasmodics (antispasmodic therapies) (1).
Surgery. Surgery involves removing your entire colon and rectum (proctocolectomy), and can eliminate ulcerative colitis (1).
Cancer surveillance. As ulcerative colitis patients have increased risk of colon cancer, you will need more-frequent colon cancer screening. However, individuals with proctitis should not worry, as they don`t have increased risk of colon cancer (1).
Ulcerative Colitis Diet, Lifestyle Tips, Supplements, Alternative Medicine and Herbal Remedies for Ulcerative Colitis
Some changes in your lifestyle and diet may help manage your symptoms and lengthen remissions.
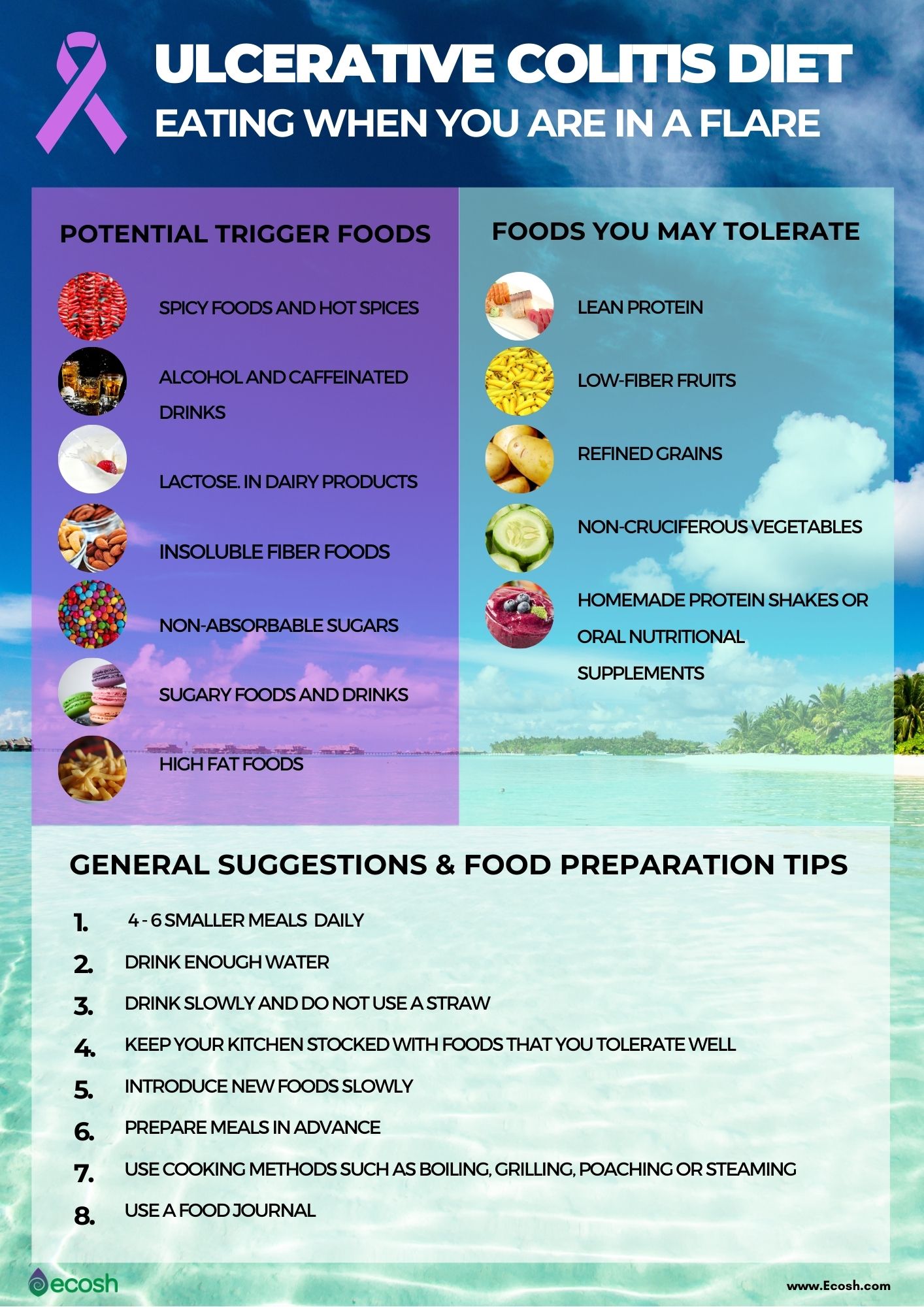
Ulcerative colitis diet. Certain foods and beverages may make your symptoms worse, some other foods on the other hand can be easier to digest and these may provide you with the right proportion of nutrients, vitamins, and minerals without worsening your symptoms. If you find out that certain foods are causing your symptoms to flare, you can try eliminating them. However consult your doctor or dietitian before starting any elimination diet. Some general dietary suggestions and food preparation tips that may help you control your disease include:
- Smaller meals. Consider eating 4 to 6 smaller meals daily rather than two or three larger ones.
- Drink enough. If your body is hydrated enough your urine should be light yellow to clear. Drink water, rehydration solution, broth, or tomato juice.
- Drink slowly and do not use a straw, as you may ingest air, which can cause gas.
- Keep your kitchen stocked with foods that you tolerate well (see list below).
- Introduce new foods slowly.
- Prepare meals in advance.
- Use healthy and simple cooking methods such as boiling, grilling, poaching or steaming.
- You can use a food journal that helps you keep track of what you eat and any symptoms that might occur due to food that you might not tolerate well (23).
During flare-up, limit or avoid:
- Spicy foods and hot spices.
- Alcohol and caffeinated drinks. Soda, coffee and all beverages containing alcohol such as beer, wine, liquor, whiskey, and vodka.
- Lactose. Dairy products that contain lactose, such as milk, cream cheese, and soft cheeses.
- Insoluble fiber foods. Raw green vegetables (particularly cruciferous vegetables like cauliflower, broccoli, or everything with a peel), whole nuts, whole grains, and fruits with skin and seeds. These foods are hard to digest.
- Non-absorbable sugars. Mannitol, sorbitol, and other sugar alcohols found in candy, sugar-free gum, ice cream, and some types of fruits and juices like peach, pear, and prune.
- Sweet and sugary foods and drinks. Juices, candy, and pastries.
- In addition, high fat foods. Margarine, butter, coconut, cream, and other greasy, fatty, and fried food
Foods that you may tolerate during flare-up include:
- Lean protein. Fish, lean meats such as lean cuts of pork, and white meat poultry, eggs, soy, and firm tofu
- Low-fiber fruits. Honeydew melon, bananas, cantaloupe, and cooked fruits. These are usually suggested for individuals who have had a recent surgery or have strictures.
- Refined grains. Potato or gluten-free bread, sourdough, white pasta, white rice, and oatmeal
- Non-cruciferous vegetables. Asparagus tips, cucumbers, squash, and potatoes. These should be consumed fully cooked, skinless and seedless.
- In addition, homemade protein shakes or oral nutritional supplements. See the list of recommended supplements above and consult your dietitian or doctor about what supplements may fit your nutritional needs (1, 4).
Lifestyle tips. Stress in one of the factors that can make your symptoms worse and trigger flare-ups. Here are some tips to help manage stress:
- Exercise. Even moderate exercise may help relieve stress, reduce depression and normalize bowel function.
- Regular relaxation and breathing exercises. Taking yoga or meditation classes, or practicing these therapies at home using books, CDs or DVDs might be an effective way to perform breathing exercises and relaxation that can help manage your stress
- Biofeedback. This is a mind-body stress-reduction technique that involves using visual or auditory feedback machines to gain control over involuntary bodily functions such as blood pressure, blood flow, and heart rate. Therefore, biofeedback may help you to reduce muscle tension, slow your heart rate, and enter a relaxed state so that you can cope more easily with stress (1).
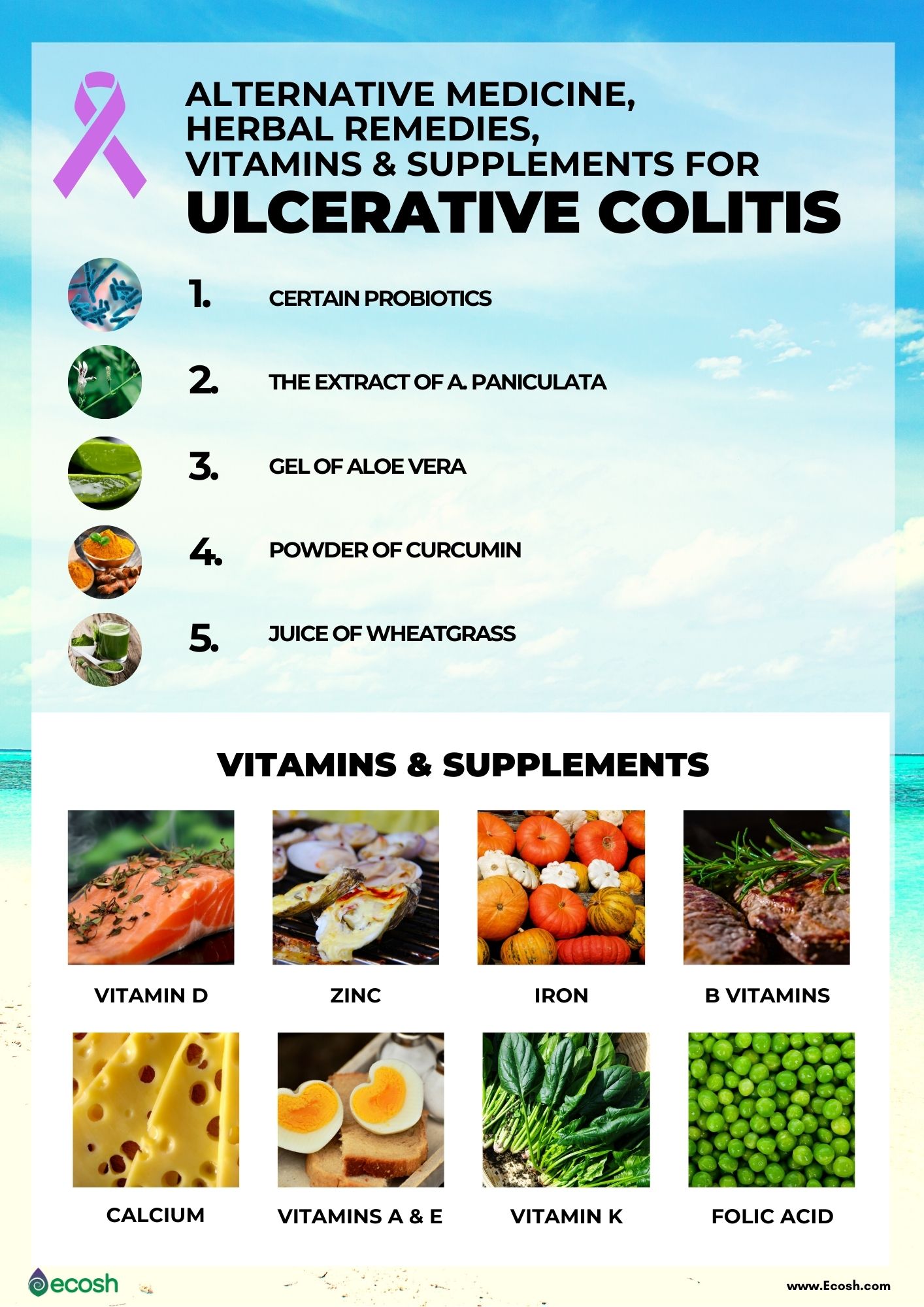
Supplements for ulcerative colitis. Severe symptoms, flare-ups, surgeries, and other complications may make it difficult for some individuals with ulcerative colitis or Crohn’s disease to get enough nutrients from food alone. Therefore, your doctor may suggest you to take some supplements. Common supplements recommended for IBD and ulcerative colitis patients include:
Iron. Iron deficiency (anemia) is a frequent complication in ulcerative colitis patients. However, only people with ulcerative colitis or Crohn’s disease that are in remission (or those without symptoms and without inflammation of the intestine) can take oral iron supplements. If you have ulcerative colitis or Crohn’s disease that is not in remission, or you cannot tolerate oral iron, intravenous iron therapy is been usually recommended (1, 5, 6, 7, 10, 16).
Vitamin D. Vitamin D is necessary for maintaining normal levels of calcium and phosphorus in the blood, which strengthen bones and prevents osteoporosis. However, according to research, almost 50% people with IBD diseases such as Ulcerative colitis and Crohn’s disease have lower vitamin D concentrations compared with healthy people. Even more, according to a study, lower levels of vitamin D in the blood may increase the risk of clinical relapse in patients with ulcerative colitis. Therefore, adding vitamin D into the diet may help reduce symptoms and increase immune system health in people with Crohn’s (10, 13, 14,16).
Vitamin B-12. This vitamin is necessary for producing new cells, protecting nerve cells, helping to make red blood cells, breaking down proteins and fats in the body. However, people with ulcerative colitis often suffer not only from vitamin B-12 deficiency, but also B-6, and B-1 deficiency (10, 14, 15).
Folic Acid. Certain inflammatory bowel disease (IBD) medications, such as methotrexate and sulfasalazine, may interfere with the absorption of folic acid. Therefore, your doctor may suggest you to take a folate supplement (10, 16).
Calcium. Intestinal inflammatory processes reduce the absorption of sodium, chloride and calcium, while they increase potassium secretion. Also, some inflammatory bowel disease (IBD) drugs (steroids) may weaken your bones. Moreover, if you cannot digest milk or milk products, you’re at even higher risk to develop calcium deficiency. Therefore, your doctor may recommend you to take calcium supplements to keep your bones healthy and prevent other problems like osteoporosis. However, for strong bones, and in order to absorb calcium, you also need vitamin D (10, 16).
Vitamins A, E, and K. If you had surgery on your intestines, it can make it hard for your body to absorb fats, which also lowers your levels of vitamins A, E and K. So you might need to take supplements or eat foods rich in these vitamins (10).
Zinc. Inflammatory bowel disease (IBD) patients with serum zinc deficiency are more likely to have adverse disease-specific outcomes. Therefore, your doctor may suggest a daily supplement to raise your levels (10, 17).
Alternative Medicine. As IBD medications can have severe side effects, some patients turn to alternative medicine. However, do not start to self medicate and consult your doctor or review the literature carefully before taking any probiotic supplements, as there is not enough scientific evidence just yet.
Probiotics. Some researchers suspect that probiotics, which are the good bacteria, might be beneficial in ulcerative colitis treatment. However, it is very important to note that not all probiotics are the same. According on the clinical trial proof available to date, only E. coli Nissle and VSL#3 seem to be efficient in controlling ulcerative colitis symptoms.
- Escherichia coli Nissle, is a strain of E. coli that has been demonstrating to be effective in promoting remission in UC patients and in addition, maintaining remission for at least 1 year.
- VSL#3 (VSL Pharmaceuticals, Inc.) which is a combination of 8 probiotics: Bifidobacterium breve, B. longum, B. infantis, Lactobacillus acidophilus, L. plantarum, L. paracasei, L. bulgaricus, and Streptococcus thermophilus. Like the trials of E. coli Nissle, trials of VSL#3 have shown efficacy for inducing remission in ulcerative colitis. Although there has not yet been a long-term maintenance trial with VSL#3, available studies have demonstrated that VSL#3 induced remission and maintained a benefit over 24 weeks (1, 8, 9, 16).
Herbal remedies. According to a 2019 review several natural herbs may reduce ulcerative colitis symptoms and significantly increase the remission. However, there are few well-designed studies about this topic just yet, and the authors of this review do not recommend any of these substances as a standalone treatment. These herbs include:
NB! The information provided here is for informational purposes only, so do not consider it as health care or medical diagnosis and treatment. Do not consider this information as a guarantee of the results you want to achieve. In addition, this information is not intended to replace the advice of your physician or other healthcare professional.
Even more, you should not use it to diagnose or treat a health problem. Before changing or discontinuing your existing medication, treatment, or care, or taking any dietary supplements, be sure to consult with your healthcare professional or doctor before starting any diet or program, or if you suspect you may have a medical condition.
Compiled by Maria-Helena Loik
Pictures: Pexels.com, Pixabay.com, Shutterstock.com
Sources:
- Ulcerative colitis – Diagnosis and treatment – Mayo Clinic
- Ulcerative colitis – NHS (www.nhs.uk)
- Types of Ulcerative Colitis | Crohn’s & Colitis Foundation
- What Should I Eat? | Crohn’s & Colitis Foundation
- ANEMIA | Crohn’s & Colitis Foundation
- Management of iron deficiency anemia in inflammatory bowel disease – a practical approach (nih.gov)
- Micronutrient deficiencies in inflammatory bowel disease – PubMed (nih.gov)
- Probiotics for Ulcerative Colitis: Do They Work? (healthline.com)
- Probiotics in the Management of Ulcerative Colitis (nih.gov)
- Vitamin and Mineral Supplementation | Crohn’s & Colitis Foundation
- Ulcerative Colitis – StatPearls – NCBI Bookshelf (nih.gov)
- Ulcerative colitis – Wikipedia
- Low level vitamin D during remission contributes to relapse in ulcerative colitis patients: Translational study suggests higher vitamin D level may benefit ulcerative colitis patients — ScienceDaily
- Micronutrient deficiencies in inflammatory bowel disease – PubMed (nih.gov)
- Vitamin B12 deficiency and IBD | IBDrelief
- Ulcerative Colitis Vitamins and Supplements (webmd.com)
- Zinc Deficiency is Associated with Poor Clinical Outcomes in Patients with Inflammatory Bowel Disease (nih.gov)
- Natural remedies for ulcerative colitis (medicalnewstoday.com)
- Phytotherapies in inflammatory bowel disease (nih.gov)


