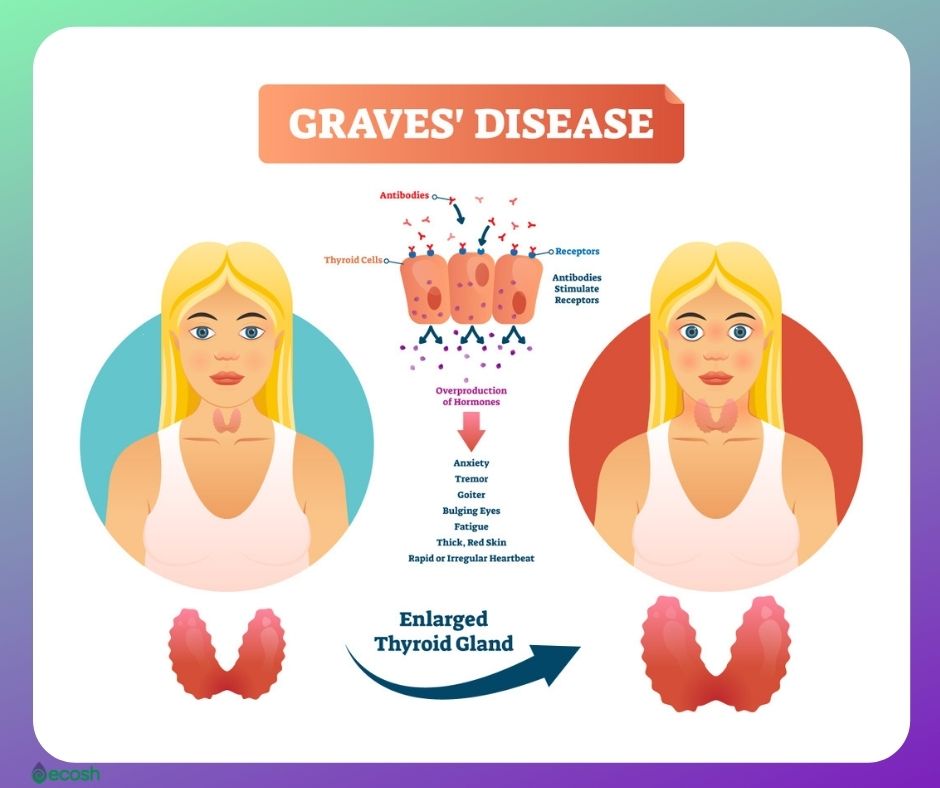
Graves’ disease is an autoimmune disorder that affects about 1 in 200 people, and is the most common cause of overactive thyroid (hyperthyroidism). Meaning, in Graves’ disease, your immune system attacks the thyroid and causes it to produce way more thyroid hormone than your body actually requires.
The thyroid, which is a butterfly-shaped gland that`s located low on the front of the neck below your Adam’s apple, wrapped around the windpipe (trachea), controls your metabolism with a few specific hormones which are created by the thyroid and tell your body’s cells how much energy to use.
Therefore, thyroid hormones affect just about every organ in your body, even the way your heart beats (1).
Without treatment, hyperthyroidism may lead to severe complications with the heart, bones, muscles, menstrual cycle, fertility, and cause health problems for the mother as well as for the baby during pregnancy. Graves’ disease also can affect your eyes (also called Graves’ eye disease, Graves’ ophthalmopathy or Graves’ orbitopathy) or/and skin (Graves’ dermopathy).
Graves’ disease is a serious health condition and needs to be treated by your healthcare provider. However, along with conventional treatment you may find help in some vitamins, lifestyle changes, home remedies, and changes in diet.
Graves’ Disease Signs and Symptoms
Common signs and symptoms of Graves’ disease include:
- Fast and irregular heartbeat (palpitations)
- Anxiety, nervousness and irritability
- Trembling hands or fingers
- Heat intolerance and an increase in perspiration or warm
- Moist skin
- Weight loss, despite normal eating habits
- Change in menstrual cycles
- Reduced libido or erectile dysfunction
- Diarrhea or frequent bowel movements
- Fatigue
- Trouble sleeping
- Tiredness or muscle weakness
- Goiter (enlargement of the thyroid gland)
- In addition, Graves’ dermopathy (reddish thickening of the skin usually on the shins or tops of the feet. This skin problem is usually painless and mild, but it can be painful for some) (1, 2).
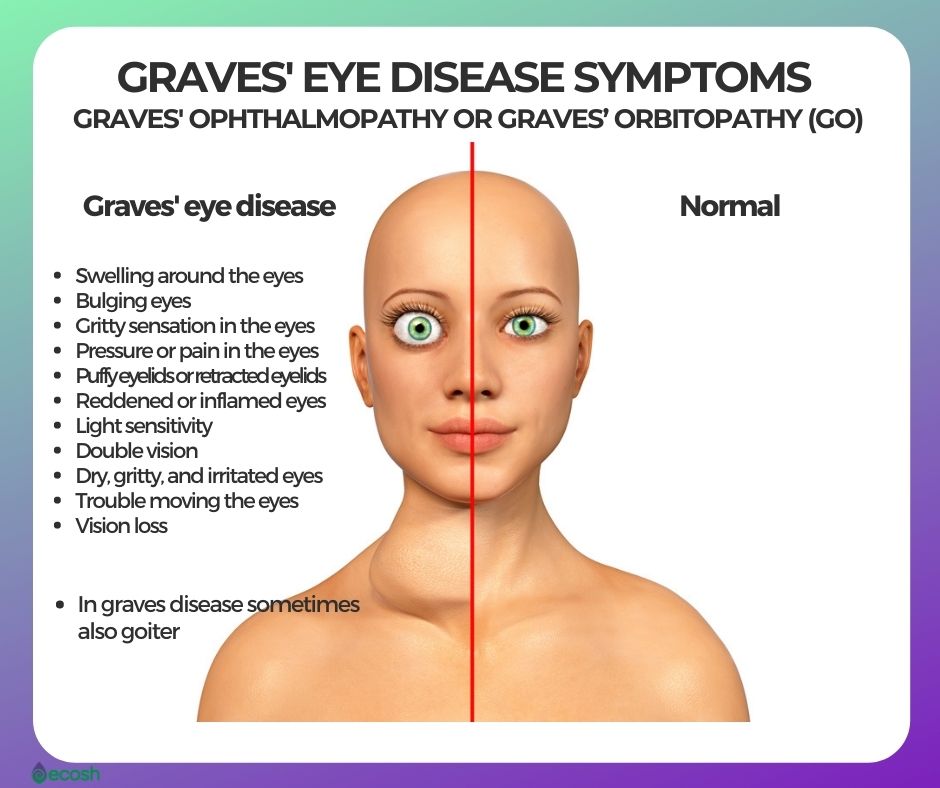
Graves’ Eye Disease (Graves’ Ophthalmopathy or Graves’ Orbitopathy (GO)) Signs and Symptoms
Around 30 percent of individuals with Graves’ disease show some signs of Graves’ ophthalmopathy, in which inflammation and other immune system events influence muscles and other tissues around your eyes. Signs and symptoms may include:
- Swelling around the eyes
- Bulging eyes
- Gritty sensation in the eyes
- Pressure or pain in the eyes
- Puffy eyelids or retracted eyelids, which means the eyelids are pulled back from the eye.
- Reddened or inflamed eyes
- Light sensitivity
- Double vision
- Dry, gritty, and irritated eyes
- Trouble moving the eyes
- Vision loss (1, 2).
Graves’ Disease Causes
Graves’ disease is autoimmune disorder caused by a malfunction in the body’s immune system. Normally, the immune system makes antibodies designed to attack a certain virus, bacterium or other foreign invader.
With Graves’ disease, the immune system produces an antibody called thyroid-stimulating immunoglobulin (TSI) that attaches to thyroid cells. TSI has a similar effect to thyroid-stimulating hormone (TSH), a hormone made in the pituitary gland that tells the thyroid how much thyroid hormone to make.
TSI causes the thyroid to produce excess thyroid hormones. It is still not entirely sure why this happens, but Graves’ disease may probably develop due to a mixture of environmental factors, genes and some outside triggers, such as for example a virus.
The onset of Graves’ disease may be triggered by physical or emotional stress, infection or giving birth (1, 5).
Causes of Graves’ Eye Disease (Graves’ Ophthalmopathy or Graves’ Orbitopathy (GO))
Graves’ eye disease happens when the immune system attacks the muscles and other tissues around the eyes, and the causes of it are unknown. However, it seems that the same antibody that can cause dysfunction of thyroid may also have an effect on tissues surrounding the eyes.
Graves’ eye disease frequently develops at the same time as hyperthyroidism or several months later, and some symptoms and signs of this disease may occur years before or after the onset of hyperthyroidism. Therefore, rarely, but sometimes, eye problems may develop long after Graves’ disease has been treated. Graves’ eye disease may even occur in people whose thyroid function is normal.
Graves’ eye disease can also develop even if there’s no hyperthyroidism.
Eye problems in Graves’ eye disease result from the swelling of tissues, muscles and fat in the socket behind the eye, which are caused by inflammation and a buildup of some carbohydrates in the tissues and muscles behind the eyes. This swelling causes exophthalmos, an unusual protrusion (bulging or protruding eyeballs) of the eye. In rare cases, inflammation is severe enough to compress, or push on, the optic nerve that leads from the eye to the brain, causing vision loss.
Graves’ eye disease has an annual adjusted incidence rate of 16 women and 3 men per 100,000 population. About one in three individuals with Graves’ disease develop mild GO, and about 5 percent develop severe GO. This eye condition usually lasts 1 to 2 years and often improves on its own (1, 2, 6, 7).
Graves’ Disease Risk Factors and Risk Groups
Anyone can develop Graves’ disease, however, many factors may increase the risk of disease, including:
Genetics. A person’s chance of developing Graves’ disease increases if other family members have the disease, as family history of Graves’ disease is a known risk factor.
Gender. Graves’ disease is seven to eight times more frequent among women than men.
Age. Graves’ disease usually develops in people between ages 30 and 50, but it can occur at any age.
Physical or emotional stress. Illnesses and stressful life events may trigger the onset of Graves’ disease among individuals who have genes that increase their risk.
Pregnancy. Being pregnant or giving birth may increase the risk of the Graves’ disease, especially among women who have genes that increase their risk.
Smoking. Cigarette smoking can influence the function of your immune system, therefore, it also increases the risk of Graves’ disease as well as Graves’ eye disease (Graves’ ophthalmopathy) among people who have Graves’ disease.
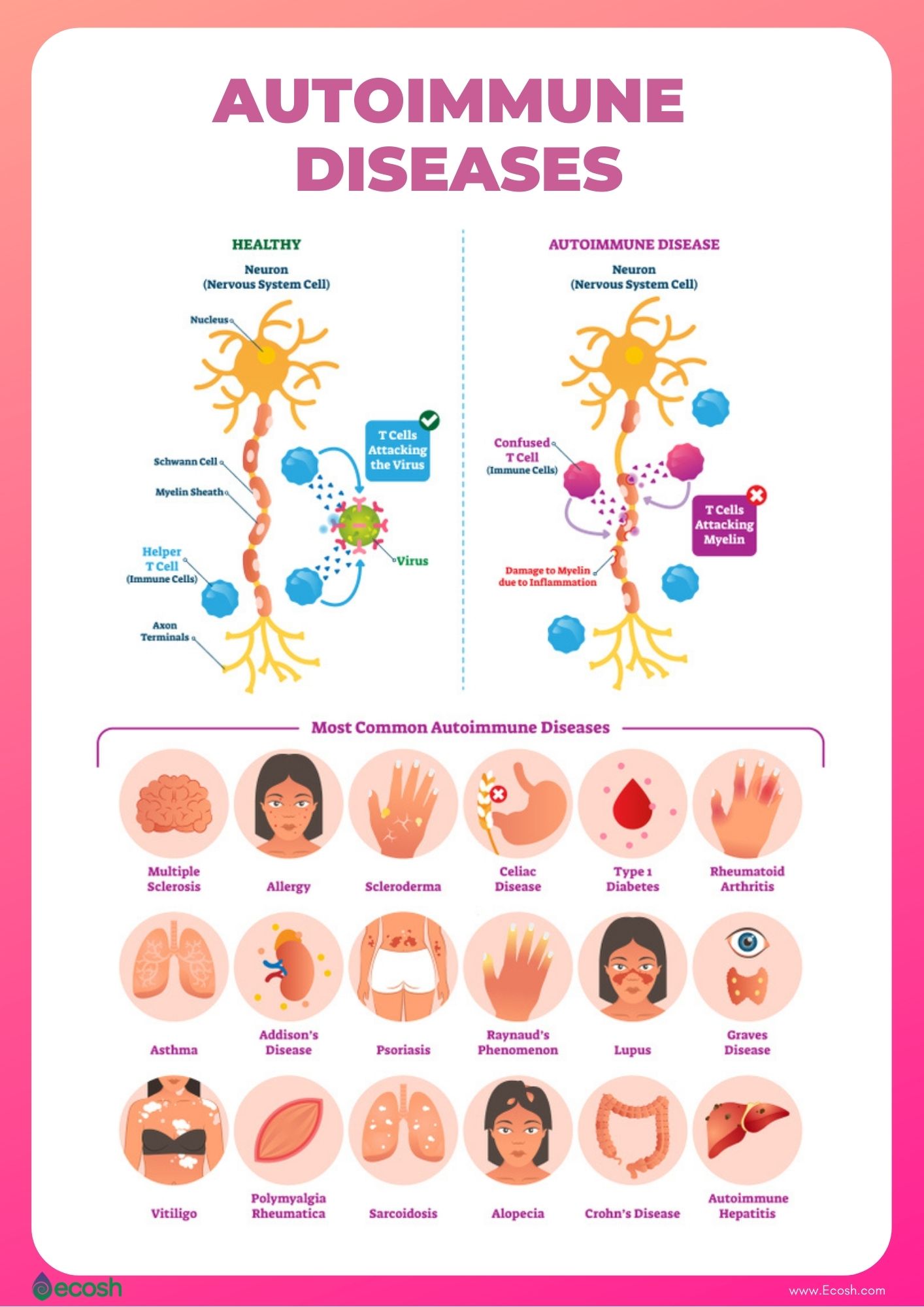
Autoimmune disorders. Individuals who have other autoimmune disorders have higher risk to develop Graves’ disease than people without these conditions. Conditions linked with Graves’ disease include:
- Rheumatoid arthritis (chronic inflammatory autoimmune disease which occurs when your body’s immune system mistakenly sends antibodies to the lining of your joints, and attacks its own healthy body tissue).
- Pernicious anemia (health disorder caused by vitamin B12 deficiency).
- Lupus (autoimmune disease that causes inflammation which can affect different bodily tissues such as for example heart, skin, joints, kidneys, blood cells, brain and lungs).
- Addison’s disease (a hormonal disorder).
- Celiac disease (a digestive disorder).
- Vitiligo (a disorder that causes skin to lose its pigmentation).
- Type 1 diabetes (1, 2).
Graves’ Disease Complications
If left untreated, Graves’ disease may cause some severe health problems, such as:
Heart problems. Graves’ disease may cause:
- Heart rhythm disorders (irregular heartbeat) that can lead to blood clots, stroke, and other heart-related problems.
- Troubles in the work and structure of the heart muscles
- Heart failure (when the heart is not pumping enough blood to the body)
Graves’ ophthalmopathy or Graves’ orbitopathy (GO). This eye disease can cause:
- Retracted eyelids
- Bulging eyes
- Double vision
- Light sensitivity
- Eye pain
- Rarely, it can also lead to vision loss
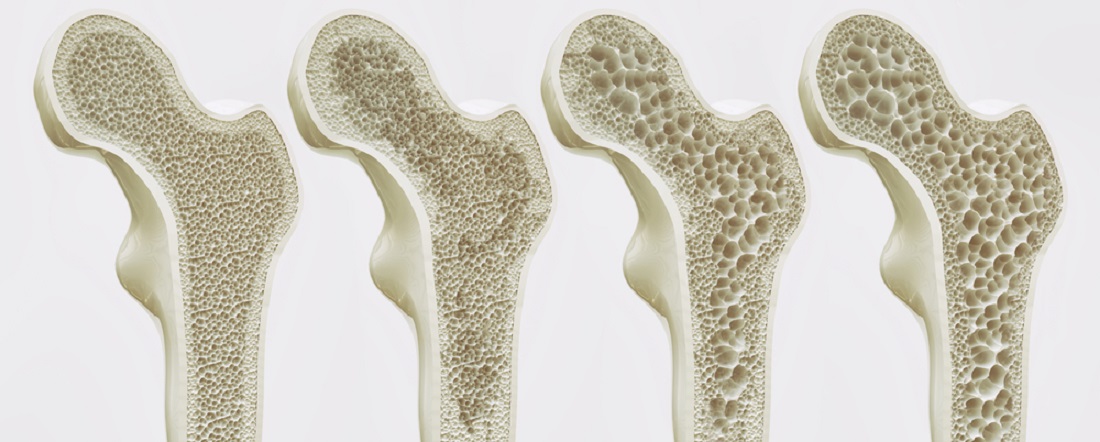
Osteoporosis, and brittle bones. Without treatment, hyperthyroidism also can lead to weak, thinning and brittle bones (osteoporosis), as too much thyroid hormone interferes with your body’s ability to absorb calcium into your bones.
Thyroid storm (accelerated hyperthyroidism or thyrotoxic crisis). This rare but life-threatening complication of Graves’ disease needs immediate emergency care, and is more likely when severe hyperthyroidism is left untreated or treated inadequately. The instant and drastic rise in thyroid hormones can produce many consequences, such as:
- Sweating
- Fever
- Vomiting
- Diarrhea
- Delirium
- Severe weakness
- Seizures
- Irregular heartbeat
- Yellow skin and eyes (jaundice)
- Severe low blood pressure
- Coma
Pregnancy problems. Usually, thyroid hormone levels that are just a little escalated are not a problem in pregnancy. However, untreated and more severe hyperthyroidism may affect the mother as well as the baby. Therefore, in case Graves’ disease, first assure your hyperthyroidism is under control before becoming pregnant. Possible complications of Graves’ disease during pregnancy include:

Graves’ Disease Treatment – Conventional Treatment, Alternative Medicine, Diet, Supplements, Lifestyle and Home Remedies
Conventional Treatment for Graves’ Disease
Factors such as your age, whether you are pregnant, or whether you have other medical conditions will determine which one out of the three treatment options (radioiodine therapy, medicines and thyroid surgery) is right for you (1).
Radioiodine therapy. In this most common treatment for Graves’ disease in the US, patients take radioactive iodine-131 as a capsule or liquid. Although the dose of I-131 usually used for radioiodine therapy does not affect other body tissues, almost everyone who has radioactive iodine treatment later develops hypothyroidism (underactive thyroid), as the thyroid hormone-producing cells have been destroyed. However, underactive thyroid disease (hypothyroidism) is much easier to treat and it causes less long-term health problems than overactive thyroid (hyperthyroidism). Individuals with hypothyroidism can perfectly manage the disease with daily thyroid hormone medicine. Radioiodine therapy is not being used if you are pregnant or are breastfeeding, because radioactive iodine can harm the fetus’ thyroid and can be passed from mother to child in breast milk (1).
Medicines. Although radioiodine therapy is the most common treatment for Graves’ disease, doctors are starting to use medicines more often than in the past.
- Beta blockers. These medicines don’t stop your thyroid from producing thyroid hormone but may lessen symptoms (such as trembling, rapid heartbeat, and nervousness) until other treatments take effect (1).
- Antithyroid medicines. These medicines cause your thyroid to produce less thyroid hormone, and are therefore the simplest treatment option for hyperthyroidism. The total average treatment time is about 12 to 18 months, but treatment can continue for many years in people who don’t want radioiodine or surgery to treat their Graves’ disease. Although antithyroid medicines usually don’t cure hyperthyroidism permanently, in some patients, the effects last a long time after they stop taking the medicine (1). As antithyroid medicine may be less harmful for the baby than other treatments, it is usually used to treat pregnant and breastfeeding women. Although these medicines may also affect the fetus, any effects are less harmful than having uncontrolled hyperthyroidism during pregnancy (1). As in some patients, antithyroid medicines may cause side effects such as allergic reactions such (rashes and itching), a decrease in the number of white blood cells in your body (that can lower resistance to infection) and in rare cases liver failure, contact your doctor immediately if you have any of the symptoms such as fever, sore throat, tiredness, weakness, dull pain in your abdomen, loss of appetite, skin rash or itching, easy bruising, yellowing of your skin or whites of your eyes, called jaundice, or constant sore throat (1).
Thyroid surgery. Sometimes surgery to remove the thyroid gland is used to treat patients with large goiters, or pregnant women who are allergic to or have side effects from antithyroid medicines. After surgery to remove your thyroid, you will develop hypothyroidism and need to take thyroid hormone medicine every day for life (1).

Alternative Medicine, Diet, Supplements, Lifestyle and Home Remedies for Graves’ Disease
If you have Graves’ disease, your physical and mental well-being should be a priority, as a healthy lifestyle may escalate the improvement in some symptoms during treatment and help you feel better in general.
Alternative Medicine, Lifestyle and Home Remedies
- Exercise. As your thyroid manages your metabolism, you may have a tendency to gain weight after the treatment when the hyperthyroidism is corrected. Graves’ disease may also influence your skeleton and cause brittle bones. Therefore weight-bearing exercises can help maintain bone density (2).
- Relieve stress. Stress may onset Graves’ disease or make it worse. Therefore, listening to your favorite relaxing music, walking in nature or taking a warm bath may help relax you and put you in a better mood. Partner with your doctor to develop a plan that involves including good nutrition, exercise and relaxation into your daily routine (2).
- Acupuncture. There’ve been few studies looking at the effectiveness of acupuncture for treating thyroid disease, but a 2018 overview of such research found several to be promising (22, 23, 24).

Graves’ Disease Diet and Supplements for Graves’ Disease
Low iodine diet. In case Graves’ disease you may be sensitive to harmful side effects from iodine, as excess iodine in your diet can escalate the production of thyroid hormone and cause or worsen hyperthyroidism. Therefore, try to avoid eating foods or taking supplements that have large amounts of iodine (such as kelp, dulse, or other types of seaweed and also some cough syrups and multivitamins). In American Thyroid Association page you will find low iodine diet tips to follow. Low in iodine diet includes foods and drinks such as:
- non iodized salt,
- egg whites,
- vegetables (fresh or frozen), vegetable oils and fruits,
- drinks such as tea, black coffee, soda, lemonade, fruit juices, beer and wine,
- herbs and spices,
- honey, sugar, jam, and jelly,
- unsalted nuts and nut butter,
- in addition, beef, chicken, turkey, veal, and lamb (moderate servings) (1, 9, 10).
Avoid allergens. In case food intolerance (even if it’s a mild one) you may want to avoid that food to lessen any adverse effects. The results that certain food allergens have on your body can mimic Graves’ disease symptoms. Therefore, removing those foods from your diet can help your doctor find out what precisely your Graves’ disease symptoms are. Most common food allergens include wheat-based foods (gluten), dairy products, soy, corn, and nuts (18).
Avoid caffeine. Caffeine content in your drinks or foods (coffee, soda, tea, and chocolate) may make the symptoms of hyperthyroidism, such as anxiety, nervousness, rapid heart rate, and weight loss – worse (11, 18).
Cruciferous vegetables. Some vegetables include compounds that lessen production of thyroid hormone. Although these foods can’t treat Graves’ disease solely, these may reduce iodine uptake by the thyroid, and be beneficial in case hyperthyroidism. Try to eat 1 or more servings every day. For instance, cruciferous vegetables include:
Berries. As in Graves’ disease your immune system attacks healthy tissues in your body – eating anti-inflammatory and antioxidant rich foods, that help keep your immune system strong may be beneficial. Although these foods can’t prevent Graves’ disease, they may help protect your overall health. Try to eat 1 or more servings fresh or frozen berries (in particular, blackberries, blueberries, and raspberries) a day (18).
Calcium. Untreated Graves’ disease may cause troubles with bone mineral density, which may lead to osteoporosis. However, calcium and vitamin D are both nutrients that are essential for your bone health and may prevent osteopenia and osteoporosis. Try to eat 2-3 servings daily. Diet rich in calcium includes foods and drinks such as (see the full list of calcium rich foods here):
Vitamin D. Many people with hyperthyroidism suffer from vitamin D deficiency, and without sufficient amounts of vitamin D, untreated Graves’ disease can cause osteoporosis. This nutrient also supports a healthy immune system as well as brain and nervous system activities. Vitamin D also has an important role in regulating insulin levels and it contributes to cardiovascular health. Try to eat 1 or more servings daily depending upon whether your vitamin D status is within range or too low. However, only few foods (see the full list here) contain some of this vitamin, and many people cannot eat enough to meet the needs for this powerful nutrient. Therefore, your healthcare provider may suggest you take a vitamin D supplement. Vitamin D rich foods include:
Protein. As losing weight is a common symptom of Graves’ disease, consuming sufficient amounts of protein may help ensure you maintain muscle mass, and help restore muscle mass once Graves’ disease is treated. Try to eat one serving (2-3 ounces) at every meal. Some quality sources of protein include:
- chicken,
- turkey,
- beans, and nuts (18).
Omega-3 fatty acids. As your body doesn’t naturally make these fatty acids, you have to get them from food. These essential fatty acids keep your body healthy and strong. Try to eat 1 or more servings every day. Some omega-3 fatty acids rich foods include:
- salmon and other fish,
- fish oil,
- olive oil,
- walnuts (18).
Selenium. Although further studies are needed to determine weather selenium supplements can help prevent or treat thyroid disease, selenium is a trace element that plays a part in thyroid hormone metabolism and has shown promising results in some studies. Your body requires selenium for the metabolism of thyroid hormones. Therefore, the maintenance of a physiological concentration of selenium (selenostasis) through a balanced diet or, alternatively, via supplementation is essential not only to prevent thyroid disease but also to maintain overall health. In addition, according to research, selenium may help improve some of the symptoms of autoimmune thyroid disease, such as thyroid eye disease (Graves’ orbitopathy). Moreover, individuals who use anti-thyroid medications, and also take selenium supplements may reach normal thyroid levels more quickly than those who do not. However, before taking any supplements, it’s important to talk with your doctor about how much selenium may be right for you since every person is different. Selenium rich diet includes foods such as:
Spices, turmeric (especially curcumin in it) and green chilis. In addition, human and animal studies have associated certain spices, such as turmeric and green chilis, to a reduced frequency of goiter, and thyroid disease, including hyperthyroidism (11, 19, 20, 21). If you cannot consume enough curcumin with food, you can try curcumin supplements which you can buy online.
L-carnitine. In conclusion, according to research, L-carnitine is effective in both reversing and preventing symptoms of hyperthyroidism and has a beneficial effect on bone mineralization. Because hyperthyroidism depletes the body deposits of carnitine and since carnitine has no toxicity, teratogenicity, contraindications and interactions with drugs, carnitine can be of clinical use (14, 16, 17).

Graves’ Eye Disease (Graves’ Ophthalmopathy or Graves’ Orbitopathy (GO)) Treatment – Conventional Treatment, Alternative Medicine, Lifestyle and Home Remedies
As the eye problems of Graves’ disease may not become better after thyroid treatment, the doctors often treat these two problems separately.
Don’t smoke. Smoking can make the condition worse.
Eye drops to keep your eyes lubricated. Eye Drops may help relieve dryness and scratchiness at any time of the day. You can tape your eyelids shut in case your eyes don’t close completely, or use a lubricating gel at bedtime to keep the cornea from drying out. In addition, a cool compress can also provide relieving moisture.
Sunglasses to help with light sensitivity and to protect your eyes. Sunglasses help protect your eyes from the sun as well as from the wind. There are also special eyeglass lenses that may help reduce double vision.
Keep your head up when sleeping. Use higher pillows when you sleep, as keeping your head up may relieve pressure on your eyes and reduce swelling.
Taping your eyes. Sometimes, if your eyelids do not fully close, taping them shut at night can help prevent dry eyes and help sleep better.
Over-the-counter creams for swollen skin. In addition, in case Graves’ dermopathy, some creams containing hydrocortisone may help reduce swollen, red skin on your feet and shins.
If the symptoms are more serious, your doctor may suggest:
- Corticosteroids. These medications may lessen swelling behind your eyeballs. However, there might be some side effects such as fluid retention, weight gain, elevated blood sugar levels, increased blood pressure and mood swings.
- Teprotumumab (Tepezza). Although this medication is new, and its role in the management of Graves’ ophthalmopathy isn’t yet defined, it may be still used to treat Graves’ ophthalmopathy. Side effects include nausea, diarrhea, muscle spasms and elevated blood sugar levels.
- Prisms. Prisms in glasses may correct double vision for some people, which may occur due to Graves’ disease or as a side effect of surgery for Graves’ disease.
- Surgery (orbital decompression). Sometimes your doctor may suggest surgery (a procedure called orbital decompression) to improve bulging of your eyes and correct the vision changes caused by pressure on the optic nerve. This surgery makes the eye socket larger, offers your eye room to sink back to a more normal position and retracted eyelids will return to their normal position. However, possible complications of this treatment include double vision.
- Radiation therapy (orbital radiotherapy). In rare cases, doctors treat Graves’ eye disease with radiation therapy to the muscles and tissues around the eyes (1, 2, 8).
NB! The information provided here is for informational purposes only, so do not consider it as health care or medical diagnosis and treatment. Do not consider this information as a guarantee of the results you want to achieve. In addition, this information is not intended to replace the advice of your physician or other healthcare professional.
Even more, you should not use it to diagnose or treat a health problem. Before changing or discontinuing your existing medication, treatment, or care, or taking any dietary supplements, be sure to consult with your healthcare professional or doctor before starting any diet or program, or if you suspect you may have a medical condition.
Compiled by Maria-Helena Loik
Pictures: Pexels.com, Pixabay.com, Shutterstock.com
Sources:
- Graves’ Disease | NIDDK (nih.gov)
- Graves’ disease – Symptoms and causes – Mayo Clinic
- Overactive thyroid (hyperthyroidism) – Causes – NHS (www.nhs.uk)
- Graves’ disease: Symptoms, treatment, and causes (medicalnewstoday.com)
- Graves’ disease – Wikipedia
- Eye Disease (Graves’ Ophthalmopathy) – Harvard Health
- Graves’ Ophthalmopathy (nih.gov)
- Hyperthyroidism – Diagnosis and treatment – Mayo Clinic
- Best diet for hyperthyroidism: Foods to eat and avoid (medicalnewstoday.com)
- Thyroid Issues? What You Should Know About Foods and Supplements to Avoid – Health Essentials from Cleveland Clinic
- Best diet for hyperthyroidism: Foods to eat and avoid (medicalnewstoday.com)
- Concentrations of thiocyanate and goitrin in human plasma, their precursor concentrations in brassica vegetables, and associated potential risk for hypothyroidism (nih.gov)
- Selenium and Thyroid Disease: From Pathophysiology to Treatment (hindawi.com)
- Supplements and Thyroid Health: What to Know (healthline.com)
- Vitamin B12 and Vitamin D Levels in Patients with Autoimmune Hypothyroidism – Medical Principles and Practice 2020, Vol. 29, No. 4 – Karger Publishers
- A novel treatment for subclinical hyperthyroidism: a pilot study on the beneficial effects of l-carnitine and selenium – PubMed (nih.gov)
- Usefulness of l-Carnitine, A Naturally Occurring Peripheral Antagonist of Thyroid Hormone Action, in Iatrogenic Hyperthyroidism: A Randomized, Double-Blind, Placebo-Controlled Clinical Trial | The Journal of Clinical Endocrinology & Metabolism | Oxford Academic (oup.com)
- How to Eat Well When You Have Graves’ Disease – (endocrineweb.com)
- Turmeric use is associated with reduced goitrogenesis: Thyroid disorder prevalence study (nih.gov)
- Turmeric For Your Thyroid – Dr. Izabella Wentz (thyroidpharmacist.com)
- Possible protective effect of curcumin on the thyroid gland changes induced by sodium fluoride in albino rats: light and electron microscopic study – PubMed (nih.gov)
- An overview of the contribution of acupuncture to thyroid disorders – PubMed (nih.gov)
- Chinese Medicine and Acupuncture for Thyroid Disease (verywellhealth.com)
- An overview of the contribution of acupuncture to thyroid disorders – ScienceDirect


