Rheumatoid arthritis is an autoimmune disease, a chronic inflammatory disorder which occurs when your body’s immune system mistakenly sends antibodies to the lining of your joints, and attacks its own healthy body tissue. In some people, this disorder can affect more than just joints and may also damage other body systems, including the eyes, skin, lungs, blood vessels and heart.
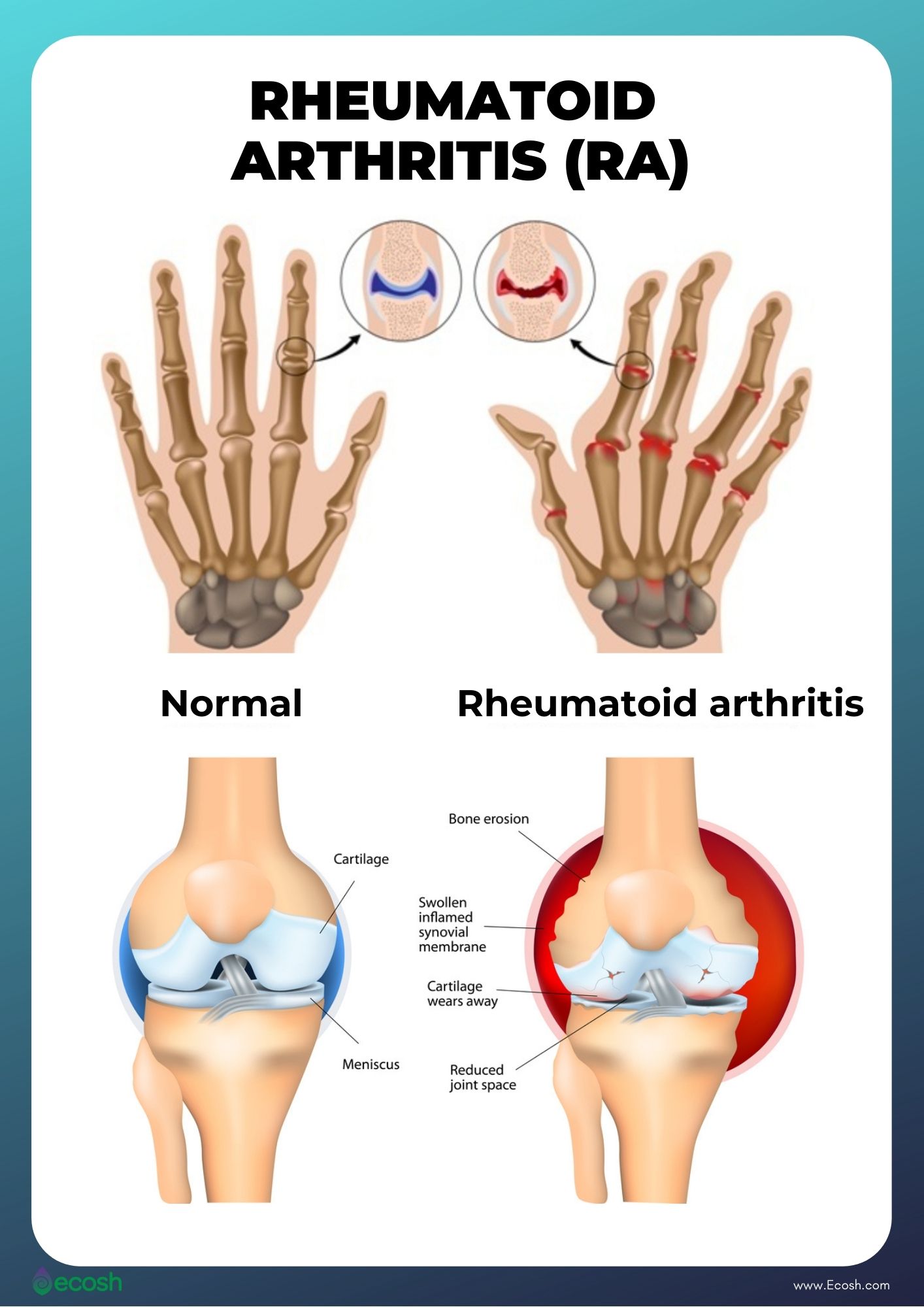
Rheumatoid arthritis affects the lining of your joints, and causes a painful swelling that can finally lead to bone erosion, joint deformity and physical disabilities (24).
Although new types of medicines have improved treatment options dramatically, in addition to medications you may find relief also in dietary changes, home remedies, and certain supplements.
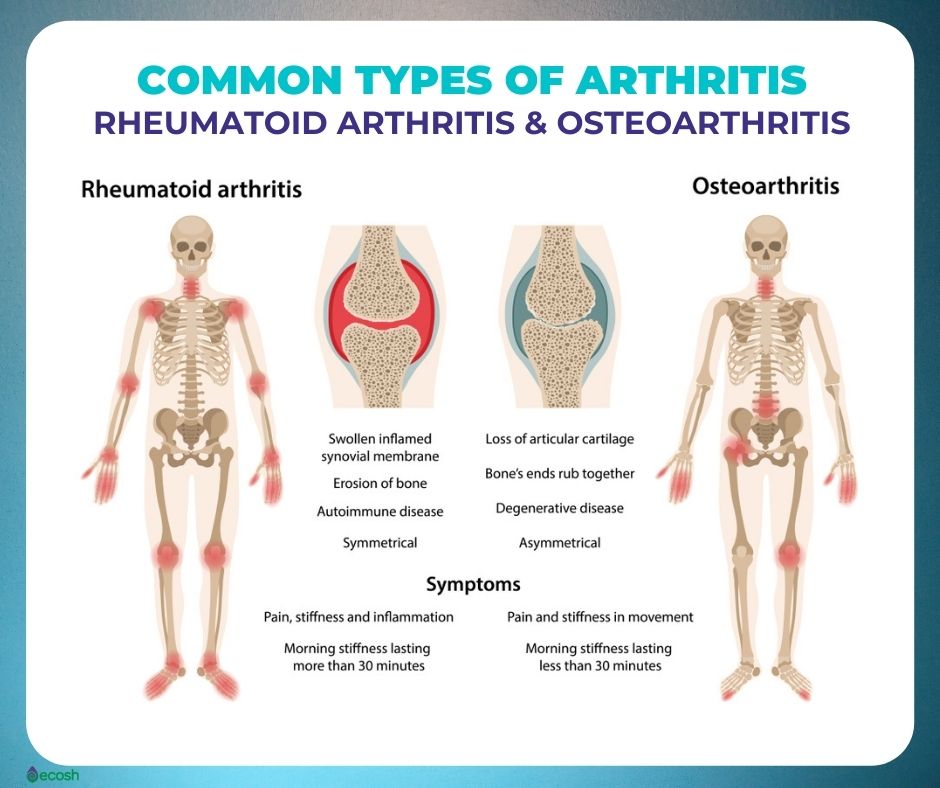
Arthritis Types
- Osteoarthritis. The most frequent type of arthritis happens when the cartilage that cushions the ends of bones in your joints gradually degenerates.
- Rheumatoid arthritis. A kind of inflammatory arthritis, known as an auto-immune health condition.
- Gout and calcium crystal diseases. A kind of inflammatory arthritis that can typically affect the big toe. But it can also affect other joints in the body and cause painful swelling.
- Spondyloarthritis. Spondyloarthritis is a word used to describe a number of conditions that cause pain and swelling, mainly around the joints of the spine. In these conditions there is inflammation of small pieces of connective tissues (entheses).
- Ankylosing spondylitis. A kind of spondyloarthritis that causes swelling and pain, mainly around the joints of the spine.
- Psoriatic arthritis. Psoriatic arthritis is a type of spondyloarthritis, and also an auto-immune condition that can cause painful stiffness and swelling within and around joints, as well as psoriasis (red scaly skin rash).
- Juvenile idiopathic arthritis (JIA). If someone is diagnosed with inflammatory arthritis before their sixteenth birthday, it’s called juvenile idiopathic arthritis, or JIA (1).
Rheumatoid Arthritis Symptoms
In case rheumatoid arthritis, sometimes symptoms might get worse (flares), and sometimes symptoms get better (remission). It can affect any joint in your body, however it is mostly felt in the small joints in the hands and feet first. Some individuals might have fleshy lumps (rheumatoid nodules that can occasionally be painful), which develop under the skin around affected joints (1, 3).
Usually, at the same time, and in the same way, both sides of the body are affected, but not always.
Rheumatoid Arthritis signs and symptoms include:
- Joint pain or aching in more than one joint
- Stiffness in more than one joint (especially first thing in the morning or after sitting still for a long time)
- Tenderness in more than one joint
- Joint swelling in more than one joint, warmth and redness
- The same symptoms and signs on both sides of your body (for instance in both knees or in both hands)
- Fatigue or tiredness, lack of energy
- Weakness
- Symptoms may also include: a poor appetite (not feeling hungry), weight loss, sweating, a high temperature or a fever, dry eyes (as a result of inflammation), chest pain (also as a result of inflammation)
- Around 40% of the rheumatoid arthritis patients also experience signs and symptoms in other places of the body that don’t involve the joints, including skin, lungs, eyes, heart, salivary glands, nerve tissue, bone marrow, blood vessels (1, 3, 24).
Rheumatoid Arthritis Causes
RA is an autoimmune disease – the result of an immune response, which means the body’s immune system mistakenly sends antibodies to the lining of your joints, and attacks its own healthy body tissue. The cells (synovium) covering your joints then become inflamed, and release chemicals that harm close by:
- bones
- cartilage
- tendons
- ligaments
If rheumatoid arthritis is left untreated, these chemicals little by little cause the joint to lose its shape and alignment. Finally, it can destroy the joint entirely.
Although there are numerous suggested theories about why the immune system mistakenly attacks the joints (for example viruses such an Epstein-Barr virus being a trigger), none of these theories has been correctly proven, and it’s not yet clear what causes this condition. However, some factors can increase the risk of developing the disease (3, 4, 8, 9).

Rheumatoid Arthritis Risk Factors and Risk Groups
There are several environmental and genetic factors that may play a role in a person’s likelihood of developing RA.
-
Age. This disease may start at any age, however the likelihood increases with age, and most people are diagnosed between the ages of 40 and 60 (1, 3).
-
Gender. New cases of rheumatoid arthritis are generally two to three times higher among women than men (1, 3).
-
Genetics/Inherited traits. Individuals with specific genes (genes called HLA (human leukocyte antigen) class II genotypes that can also make arthritis worse) have higher risk to develop RA. The likelihood to develop RA may be highest when individuals with these genes are obese or are revealed to environmental factors such as smoking (1, 3).
-
Cigarette smoking. Smoking notably increases a person’s likelihood of developing rheumatoid arthritis and can also make the disease worse (1, 3).
-
History of live births. Women who have never given birth may be at higher risk of developing rheumatoid arthritis (1, 3).
-
Diet. Diet rich in red meat, and the lack of vitamin C has been linked to increased risk of developing rheumatoid arthritis (1, 3, 6, 7).
-
Early Life Exposures. According to a study, children whose mothers smoked had double the risk of developing rheumatoid arthritis as adults. However, early initiation of breastfeeding may be protective against this disease. Also a high birth weight seems to be a risk factor for developing rheumatoid arthritis (1, 3, 5).
-
Obesity. Individuals with overweight have a significantly higher risk of developing rheumatoid arthritis. BMI (The body mass index) is most commonly used to calculate if your weight is within the normal range. An ideal BMI for adults is in the 18.5 to 24.9 range.
BMI measures (1, 3):
Rheumatoid Arthritis Treatment – Medications, Home Remedies, Diet and Supplements
There are many ways to effectively treat and manage rheumatoid arthritis such as medication(s), alternative or home remedies, diet, and specific types of exercise. The earlier you start the resolute treatment, the more likely it is to work (1, 3, 10).
Medications for Rheumatoid Arthritis Treatment:
Many people who suffer from rheumatoid arthritis need to administer more than one medication. This is because different drugs work in different ways, and many people with RA may need to take more than one drug.
- Painkillers.
- Disease-modifying anti-rheumatic drugs (DMARDs). These are medicines that prevent joint deformity and slow disease.
- Biologics. These biological response modifiers (biologicals are new generation biologic DMARDs) are medications that provide a targeted response to inflammation rather than blocking your body’s entire immune system response. They may be an efficient medication for people who don’t respond to more traditional DMARDs.
- Janus kinase (JAK) inhibitors. Your doctor may suggest these new subcategory of DMARDs (that block certain immune responses) to help prevent inflammation and stop damage to your joints when DMARDs and biologic DMARDs don’t work for you.
- Steroids (also known as corticosteroids)
- Non-steroidal anti-inflammatory drugs (NSAIDs). NSAIDs such as paracetamol, aspirin, and ibuprofen are used to relieve symptoms of arthritis, lessen pain and reduce inflammation (1, 3, 10, 11).

Home Remedies and Lifestyle Changes for Rheumatoid Arthritis Treatment:
In addition to medications, people can manage their RA with self-management strategies proven to reduce pain and disability, allowing them to pursue the activities important to them (1, 3, 10, 12).
- Maintain a healthy weight. Sustaining a healthy weight can limit arthritis development and activity restrictions, as for every pound lost, there is a 4 pound lightening in the load exerted on the knee. Therefore, for individuals who are carrying extra weight, even a modest weight loss (for example, 5% or 12 pounds for a 250 pound person) can help lessen arthritis symptoms such as pain and disability (2, 10, 12).
- Exercise. Physical activity (low-impact exercises such as gentle yoga) can help to increase the range of movement in your joints, decrease pain, delay disability and also strengthen muscles, that is important for taking off some of the pressure from your joints. Individuals with arthritis should aim to get at least 150 minutes of modest physical activity each week for considerable health benefits. You can break up the 150 minutes into shorter periods (2, 10, 12).
- Get enough rest. Your body may require more resting time during flare-ups and less during remission. Getting an adequate amount of sleep will help to lessen pain, fatigue and inflammation (10).
- Apply heat or cold. Cold compresses as well as ice packs may help to lessen the pain, inflammation and muscle spasms. Rotating cold treatments with hot therapies like hot compresses and warm showers may help to reduce stiffness (10).
- Try assistive devices and protect your joints. Specific devices like braces and splints may help to reduce inflammation as these can hold your joints in a resting position, and help avoid injuries related to work or sports. Crutches and canes can help you maintain mobility, even in the course of flares. You can also use household gadgets, for instance grab bars and handrails in bathrooms and along staircases (10, 12).

Rheumatoid Arthritis Diet
Individuals with rheumatoid arthritis usually have a greater risk of developing heart disease. Therefore, dietary changes along with prescription medications may influence blood cholesterol levels, support the overall health, improve symptoms, and might also influence the level of joint pain and inflammation.
However, a small number of people with rheumatoid arthritis may also have an intolerance to one or more foods. Therefore, to know what not to eat is just as important to know what to eat. These trigger foods can be identified through an exclusion programme under the supervision of a dietitian (2, 10, 22).
-
Oily fish. Oily fish such as for example salmon, sardines, mackerel, snapper, and herring are packed with omega-3 polyunsaturated fats. Besides their benefits for heart-health, fish oils have been shown to help lower overall inflammation and may therefore help to lessen joint pain and stiffness. Aim two portions of oily fish a week (1 portion: 140g or a small fillet) of oily fish a week, and seek for other foods enriched with omega-3 such as some eggs and breads. Omega-3 fatty acids from plant sources (GLA) are of limited benefit and have a lower effect on reducing inflammation (2, 10, 13, 14, 22).
-
Mediterranean diet. Mediterranean diet is a type of diet where saturated fats are minimized and replaced with unsaturated fats including omega-3. Diet includes poultry, fish, less lean meat that normally, plenty of vegetables (fresh, frozen or canned), fresh fruit, olive oil, wholegrain cereals, beans, peas, seeds and nuts. Although there is not enough evidence just yet – some studies have shown an improvement in some symptoms of rheumatoid arthritis when following this diet (2, 16, 22).
-
Antioxidant rich foods. Eating more antioxidant rich foods such as rich berries, fruits and vegetables (5-a-day) may help to reduce inflammation and improve symptoms of rheumatoid arthritis (2, 10, 17). Antioxidants rich foods include:
- Berries (blueberries, strawberries, cranberries, and goji berries)
- Dark chocolate
- Spinach
- Kidney beans
- Pecans
- Artichokes
-
Iron-rich foods. Being tired is a very common symptom of rheumatoid arthritis, and tiredness can be even worse if you have anaemia. Anaemia can happen as a consequence of decreased iron absorption during a ‘flare-up’. To try to help stop this, eat iron-rich foods consistently. Your body absorbs iron more easily if you have it together with vitamin C, so eat a portion of vitamin C rich foods such as fruits or vegetables with your meal (2). Iron-rich foods include:
- Blood
- Liver
- Red meats
- Fish
- Poultry
- Garden Thyme
- Dandelion
- Dock
- Plantago
- Nettle
- Raspberry
- Blueberry
- Pumpkin
- Seeds (especially poppy, sesame, sunflower, pumpkin and flax seeds)
- Legumes (beans, lentils, peas)
- Nuts (especially hazelnut)
- Dried fruits (apricots, peaches, plums, raisins)
- Red beet juice
-
Calcium-rich foods. It is important to get an adequate amount of calcium in your diet to ensure the bones stay healthy and strong. Especially when you have rheumatoid arthritis and you use glucocorticoids as part of the treatment, as it may put you at greater risk of developing osteoporosis. Calcium rich foods include (2):
- Green leafy vegetables like for example kale, spinach, turnips
- Canned salmon or fish with bones such as sardines
- Tofu, Soybeans and fortified soymilk
- Enriched breads, grains, and waffles
- Dried fruit
- Yoghurt
- Cheese
- Milk
- Fortified cereals
- Fortified orange juice (2).
-
Vegetarian diet. A vegetarian diet may potentially relieve symptoms and disease activity in some rheumatoid arthritis patients, however speak to your doctor or dietitian to make sure you are still getting enough nutrients before you try any diet (2, 22).

Supplements for Rheumatoid Arthritis Treatment
A healthy diet should usually include all the nutrients your body needs. However, if your diet is limited or your appetite is poor, some supplements may provide useful nutrients. Consult with your doctor before taking a new supplement (2).
-
Omega-3 fatty acids in fish oil. Fish oil supplements (in high doses) that contain omega-3 fatty acids have been shown to lessen the symptoms of rheumatoid arthritis, like the time of morning stiffness, the level of joint pain and the amount of swollen and tender joints. Fish oil supplements you take should have at least 500-1000mg of EPA and DHA (omega-3 fats) in one capsule. It can take almost up to 3 months for your symptoms to be relieved, so be patient. In addition, consult your doctor before taking any new supplements. (2, 13, 14, 15).
-
Vitamin D. There is some evidence that vitamin D deficiency is very common among people with rheumatoid arthritis. Vitamin D deficiency may also be linked to rheumatoid arthritis severity, it progresses more quickly and is more painful. Therefore a vitamin D supplement may be useful during winter months for the prevention of osteoporosis as well as for pain relief in patients with rheumatoid arthritis (2, 18).
-
Antioxidants. Although more research is still needed, some evidence suggests the necessity for therapeutic co-administration of antioxidants (such as for example vitamins A, C, E, and selenium) along with conventional drugs to such rheumatoid arthritis patients (2, 17).
-
Probiotics. Gut bacteria plays a vital role in immune regulation. Although the use of probiotics as a treatment for rheumatoid arthritis has not been proven, and further studies are needed, some emerging data suggest that probiotics may lower inflammation. Therefore leading researchers state that the use of probiotics may be an effective adjunct therapy for patients with rheumatoid arthritis (2, 20, 21, 22, 23).
- Curcumin. According to an animal study, curcumin may have anti-arthritic properties and it can be potentially used for the treatment of rheumatoid arthritis (15, 19, 20). Read more about the 22 scientifically proven health benefits of curcumin.
NB! The information provided here is for informational purposes only, so do not consider it as health care or medical diagnosis and treatment. Do not consider this information as a guarantee of the results you want to achieve. In addition, this information here is not intended to replace the advice of your physician or other healthcare professional.
Even more, you should not use it to diagnose or treat a health problem. Before changing or discontinuing your existing medication, treatment, or care, or taking any dietary supplements, be sure to consult with your healthcare professional or doctor before starting any diet or program, or if you suspect you may have a medical condition.
Written by Maria-Helena Loik
Photos: Pexels.com, Pixabay.com, Shutterstock.com
Sources:
- Arthritis | Causes, symptoms, treatment | Versus Arthritis
- Diet and Rheumatoid Arthritis Food Fact Sheet (bda.uk.com)
- Rheumatoid Arthritis (RA) | Arthritis | CDC
- Rheumatoid arthritis – Causes – NHS (www.nhs.uk)
- The influence of early life factors on the risk of developing rheumatoid arthritis (nih.gov)
- Vitamin C May Fight Rheumatoid Arthritis (webmd.com)
- Eating red meat may increase the risk of rheumatoid arthritis | EurekAlert! Science News
- Epstein–Barr virus and rheumatoid arthritis: is there a link? (nih.gov)
- Rheumatoid arthritis and Epstein-Barr virus: a case of living with the enemy? | Annals of the Rheumatic Diseases (bmj.com)
- Rheumatoid Arthritis: Symptoms, Causes, Treatment, and More (healthline.com)
- Painkillers and NSAIDs | Side-effects, uses, time to work (versusarthritis.org)
- Key Public Health Messages About Arthritis | CDC
- The Effect of Omega-3 Fatty Acids on Rheumatoid Arthritis (nih.gov)
- Effects of high-dose fish oil on rheumatoid arthritis after stopping nonsteroidal antiinflammatory drugs. Clinical and immune correlates – PubMed (nih.gov)
- Supplements for rheumatoid arthritis – Harvard Health
- The effects of the Mediterranean diet on rheumatoid arthritis prevention and treatment: a systematic review of human prospective studies – PubMed (nih.gov)
- Antioxidant status in rheumatoid arthritis and role of antioxidant therapy – PubMed (nih.gov)
- Vitamin D and rheumatoid arthritis (nih.gov)
- Turmeric for Rheumatoid Arthritis: Benefits and Side Effects (healthline.com)
- Probiotics for the Management of Rheumatoid Arthritis – ScienceDirect
- Do Probiotics Help Arthritis Symptoms?
- Managing Rheumatoid Arthritis with Dietary Interventions (nih.gov)
- Probiotic supplementation improves inflammatory status in patients with rheumatoid arthritis – PubMed (nih.gov)
- Rheumatoid arthritis – Symptoms and causes – Mayo Clinic



Your writing is so powerful and has the ability to make a real difference in people’s lives Keep using your voice to spread kindness and positivity
I’m often to blogging and i really appreciate your content. The article has actually peaks my interest. I’m going to bookmark your web site and maintain checking for brand spanking new information.
You’re so awesome! I don’t believe I have read a single thing like that before. So great to find someone with some original thoughts on this topic. Really.. thank you for starting this up. This website is something that is needed on the internet, someone with a little originality!
Hi there to all, for the reason that I am genuinely keen of reading this website’s post to be updated on a regular basis. It carries pleasant stuff.