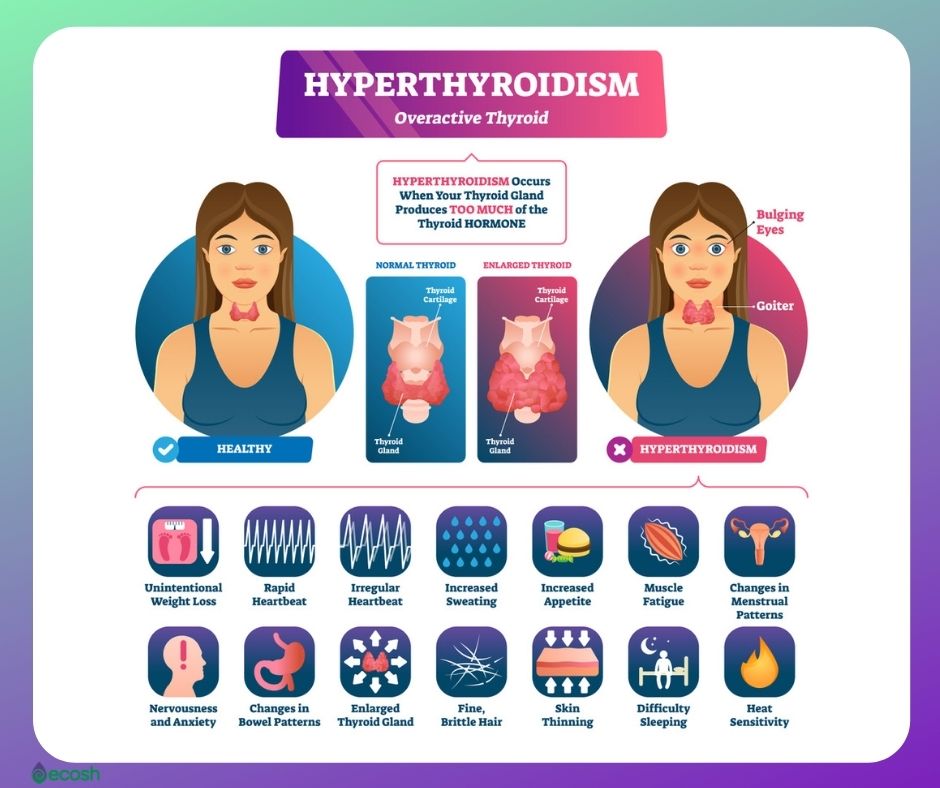
Graves’ eye disease, also called Graves’ ophthalmopathy and Graves’ orbitopathy (GO), is a potentially sight-threatening ocular disease that may develop in people with an overactive thyroid (hyperthyroidism) caused by Graves’ disease. Graves’ eye disease is also known as thyroid-associated ophthalmopathy or thyroid eye disease, because it sometimes occurs in patients with euthyroid or hypothyroid chronic autoimmune thyroiditis.
This eye disease has an annual adjusted incidence rate of 16 women and 3 men per 100,000 population (26, 27).
Eye problems in Graves’ eye disease result from the swelling of tissues, muscles and fat in the socket behind the eye, which are caused by inflammation and a buildup of some carbohydrates in the tissues and muscles behind the eyes. This swelling causes exophthalmos, an unusual protrusion (bulging or protruding eyeballs) of the eye. Moreover, in rare cases, inflammation is severe enough to compress, or push on, the optic nerve that leads from the eye to the brain, causing vision loss.
As the Graves’ eye disease may not become better after thyroid treatment, the doctors often treat these two problems separately. However, along with conventional treatment you may find help in some home remedies.
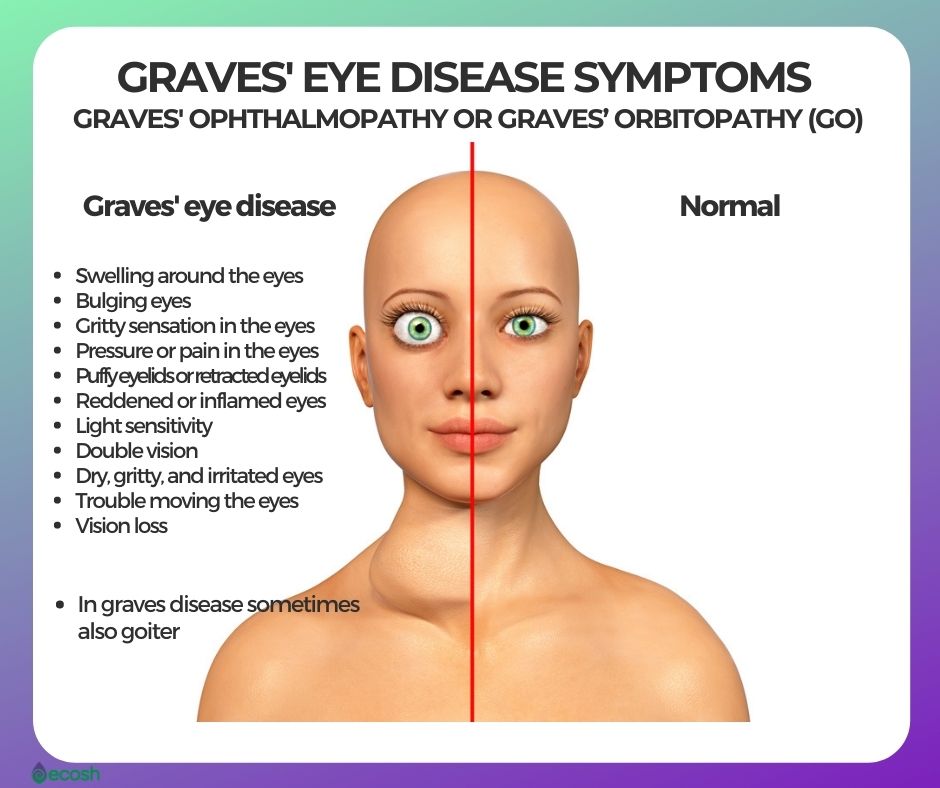
Graves’ Eye Disease (Graves’ Ophthalmopathy or Graves’ Orbitopathy (GO)) Signs and Symptoms
Around 30 percent of individuals with Graves’ disease show some signs of Graves’ ophthalmopathy, in which inflammation and other immune system events influence muscles and other tissues around your eyes. Signs and symptoms may include eye problems such as:
- Swelling around the eyes
- Bulging eyes
- Gritty sensation in the eyes
- Pressure or pain in the eyes
- Puffy eyelids or retracted eyelids, which means the eyelids are pulled back from the eye.
- Reddened or inflamed eyes
- Light sensitivity
- Double vision
- Dry, gritty, and irritated eyes
- Trouble moving the eyes
- In addition, vision loss (1, 2).
Causes of Graves’ Eye Disease (Graves’ Ophthalmopathy or Graves’ Orbitopathy (GO))
Graves’ eye disease happens when the immune system attacks the muscles and other tissues around the eyes, and the causes of it are unknown. However, it seems that the same antibody that can cause dysfunction of thyroid may also have an effect on tissues surrounding the eyes.
Graves’ eye disease frequently develops at the same time as hyperthyroidism or several months later, and some symptoms and signs of this disease may occur years before or after the onset of hyperthyroidism. Therefore, rarely, but sometimes, eye problems may develop long after Graves’ disease has been treated. Graves’ eye disease may even occur in people whose thyroid function is normal.
Graves’ eye disease can also develop even if there’s no hyperthyroidism.
Eye problems in Graves’ eye disease result from the swelling of tissues, muscles and fat in the socket behind the eye, which are caused by inflammation and a buildup of some carbohydrates in the tissues and muscles behind the eyes. This swelling causes exophthalmos, an unusual protrusion (bulging or protruding eyeballs) of the eye. In rare cases, inflammation is severe enough to compress, or push on, the optic nerve that leads from the eye to the brain, causing vision loss.
Graves’ eye disease has an annual adjusted incidence rate of 16 women and 3 men per 100,000 population. About one in three individuals with Graves’ disease develop mild GO, and about 5 percent develop severe GO. This eye condition usually lasts 1 to 2 years and often improves on its own (1, 2, 6, 7).

Graves’ Eye Disease Risk Factors and Risk Groups
Anyone with Graves’ disease can develop Graves’ eye disease, however, some factors may increase the risk, including:
- Having hyperthyroidism due to Graves’ disease. According to one study, Graves’ eye disease (Graves’ ophthalmopathy) was observed in 604 (58%) of the 1042 participants with Graves’ disease.
- Being Caucasian. In addition, according to study, the proportion of Caucasian in Graves’ disease with Graves’ eye disease (79.8%) was greater than non-GO controls (64.6%).
- Radioactive iodine therapy. Some Graves’ disease treatments such as radioactive iodine therapy may increase the risk of Graves’ eye disease.
- Smoking. Cigarette smoking can influence the function of your immune system, therefore, it also increases the risk of Graves’ disease as well as Graves’ eye disease (Graves’ ophthalmopathy) among people who have Graves’ disease (1, 2, 25).

Graves’ Eye Disease (Graves’ Ophthalmopathy or Graves’ Orbitopathy (GO)) Treatment – Conventional Treatment, Lifestyle and Home Remedies
As the eye problems of Graves’ disease may not become better after thyroid treatment, the doctors often treat these two problems separately.
-
Reversing hyperthyroidism caused by Graves’ disease. Firstly, the most important step of treatment is to reverse hyperthyroidism with medication, radioiodine therapy thyroid or surgery. Along with conventional treatment you may find help also in diet, lifestyle changes and some supplements. Read more about Graves’ disease treatment options here.
-
Don’t smoke. Secondly, try to quit smoking, as it can make the condition worse.
-
Eye drops to keep your eyes lubricated. Thirdly, use eye drops, as these lubricate your eyes, and may therefore help reduce dryness and scratchiness at any time of the day. You can also use a lubricating gel at bedtime to keep the cornea from drying out. In addition, a cool compress can also provide relieving moisture.
-
Sunglasses to help with light sensitivity and to protect your eyes. Sunglasses can provide protection from the sun as well as from the wind. There are also special eyeglass lenses that may help reduce double vision.
-
Keep your head up when sleeping. Use higher pillows when you sleep, as keeping your head up may relieve pressure on your eyes and reduce swelling.
-
Taping your eyes. Sometimes, if your eyelids do not fully close, taping them shut at night can help prevent dry eyes and help sleep better.
-
Over-the-counter creams for swollen skin. In addition, in case Graves’ dermopathy, some creams containing hydrocortisone may help reduce swollen, red skin on your feet and shins.
-
If the symptoms are more serious, your doctor may suggest:
- Corticosteroids. These medications may lessen swelling behind your eyeballs. However, there might be some side effects such as fluid retention, weight gain, elevated blood sugar levels, increased blood pressure and mood swings.
- Teprotumumab (Tepezza). Although this medication is new, and its role in the management of Graves’ ophthalmopathy isn’t yet defined, it may be still used to treat Graves’ ophthalmopathy. Side effects include nausea, diarrhea, muscle spasms and elevated blood sugar levels.
- Prisms. Prisms in glasses may correct double vision for some people, which may occur due to Graves’ disease or as a side effect of surgery for Graves’ disease.
- Surgery (orbital decompression). Sometimes your doctor may suggest surgery (a procedure called orbital decompression) to improve bulging of your eyes and correct the vision changes caused by pressure on the optic nerve. This surgery makes the eye socket larger, offers your eye room to sink back to a more normal position and retracted eyelids will return to their normal position. However, possible complications of this treatment include double vision.
- Radiation therapy (orbital radiotherapy). In conclusion, in rare cases, doctors treat Graves’ eye disease with radiation therapy to the muscles and tissues around the eyes (1, 2, 8).
NB! The information provided here is for informational purposes only, so do not consider it as health care or medical diagnosis and treatment. Do not consider this information as a guarantee of the results you want to achieve. In addition, this information is not intended to replace the advice of your physician or other healthcare professional.
Even more, you should not use it to diagnose or treat a health problem. Before changing or discontinuing your existing medication, treatment, or care, or taking any dietary supplements, be sure to consult with your healthcare professional or doctor before starting any diet or program, or if you suspect you may have a medical condition.
Compiled by Maria-Helena Loik
Pictures: Pexels.com, Pixabay.com, Shutterstock.com
Sources:
- Graves’ Disease | NIDDK (nih.gov)
- Graves’ disease – Symptoms and causes – Mayo Clinic
- Overactive thyroid (hyperthyroidism) – Causes – NHS (www.nhs.uk)
- Graves’ disease: Symptoms, treatment, and causes (medicalnewstoday.com)
- Graves’ disease – Wikipedia
- Eye Disease (Graves’ Ophthalmopathy) – Harvard Health
- Graves’ Ophthalmopathy (nih.gov)
- Hyperthyroidism – Diagnosis and treatment – Mayo Clinic
- Best diet for hyperthyroidism: Foods to eat and avoid (medicalnewstoday.com)
- Thyroid Issues? What You Should Know About Foods and Supplements to Avoid – Health Essentials from Cleveland Clinic
- Best diet for hyperthyroidism: Foods to eat and avoid (medicalnewstoday.com)
- Concentrations of thiocyanate and goitrin in human plasma, their precursor concentrations in brassica vegetables, and associated potential risk for hypothyroidism (nih.gov)
- Selenium and Thyroid Disease: From Pathophysiology to Treatment (hindawi.com)
- Supplements and Thyroid Health: What to Know (healthline.com)
- Vitamin B12 and Vitamin D Levels in Patients with Autoimmune Hypothyroidism – Medical Principles and Practice 2020, Vol. 29, No. 4 – Karger Publishers
- A novel treatment for subclinical hyperthyroidism: a pilot study on the beneficial effects of l-carnitine and selenium – PubMed (nih.gov)
- Usefulness of l-Carnitine, A Naturally Occurring Peripheral Antagonist of Thyroid Hormone Action, in Iatrogenic Hyperthyroidism | Oxford Academic (oup.com)
- How to Eat Well When You Have Graves’ Disease – (endocrineweb.com)
- Turmeric use is associated with reduced goitrogenesis: Thyroid disorder prevalence study (nih.gov)
- Turmeric For Your Thyroid – Dr. Izabella Wentz (thyroidpharmacist.com)
- Possible protective effect of curcumin on the thyroid gland changes induced by sodium fluoride in albino rats – PubMed (nih.gov)
- An overview of the contribution of acupuncture to thyroid disorders – PubMed (nih.gov)
- Chinese Medicine and Acupuncture for Thyroid Disease (verywellhealth.com)
- An overview of the contribution of acupuncture to thyroid disorders – ScienceDirect
- Risk Factors for Graves’ Orbitopathy; the Australian Thyroid-Associated Orbitopathy Research (ATOR) Study | Oxford Academic (oup.com)
- Graves’ Ophthalmopathy (nih.gov)
- Graves’ Eye Disease (Graves’ Ophthalmopathy) – Harvard Health


