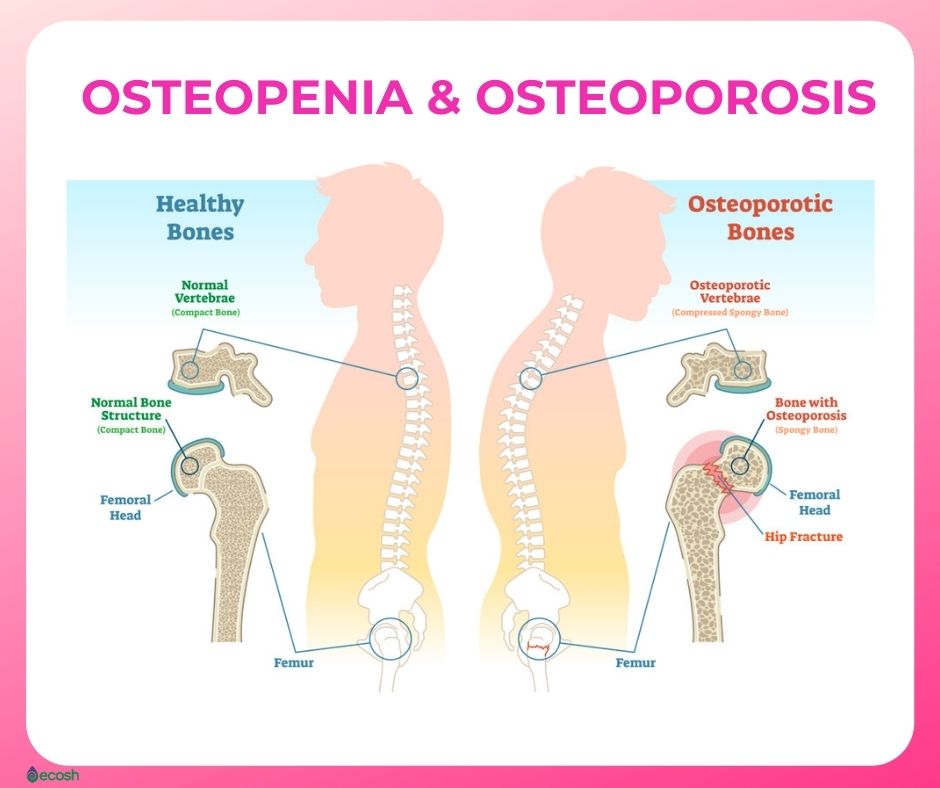
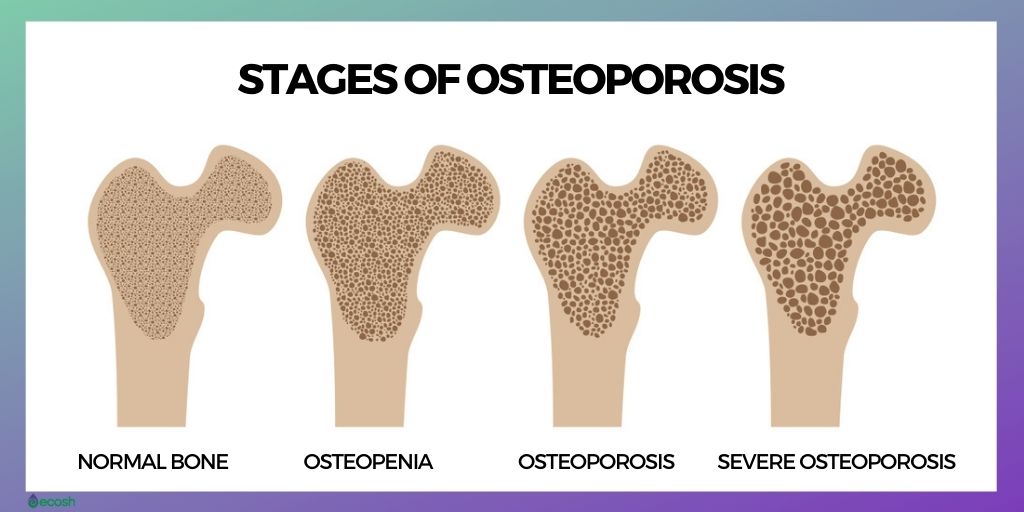
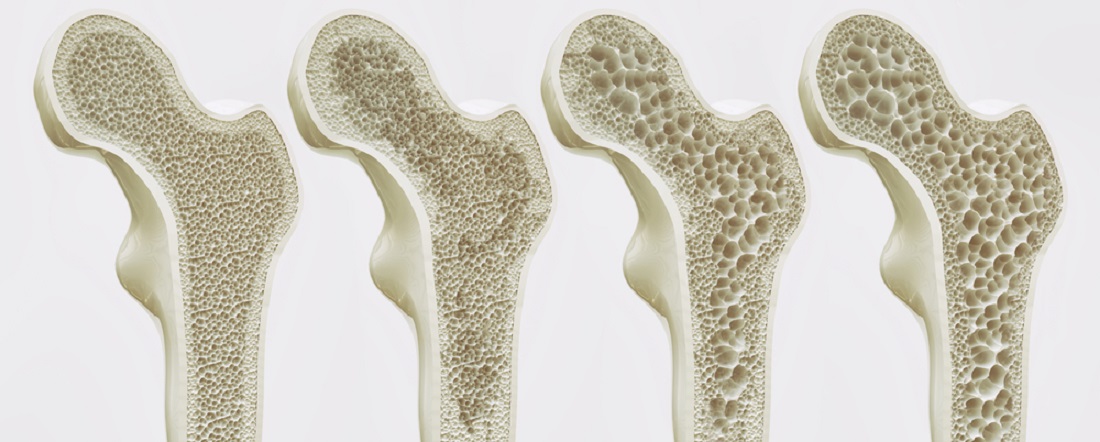
Osteopenia and osteoporosis are related diseases. Osteopenia is a stage before osteoporosis, when a bone density scan shows you have lower bone density than the average for your age, but not low enough to be diagnosed as osteoporosis.
Osteoporosis happens when your body makes too little bone or loses too much bone, or both, as bone is living tissue that is constantly being broken down and replaced. As a result, bones become weak and brittle and may break from a fall (1, 20). Osteopenia affects about half of Americans over age 50 (21).
However, although osteopenia is a big risk factor for developing osteoporosis, it does not always lead to osteoporosis. Especially when you take the steps to reduce your risk of developing osteoporosis and keep your bones healthy (4). Here are 8 tips to prevent osteopenia, osteoporosis and keep your bones healthy.
Osteopenia Symptoms
Osteopenia as well as osteoporosis do not usually cause any symptoms such as pain or movement complications on their own. This makes it difficult to detect if someone may have either condition, and the best bet for detecting osteopenia or osteoporosis in the early stages is to have a bone density test.
However, one of the most general symptoms is height loss. As people age, most of them lose an average of one inch of their height, but losing more than an inch may be the first sign that there might be a hidden bone density problem.
The biggest indicators for bone abnormality are fractures or broken bones. For example, if a person over age 50 falls from a standing height and breaks a bone, might be a clear sign of osteopenia or osteoporosis, and a bone density test should be done. Even individuals with osteopenia may be at risk for fractures and broken bones (23).
Although typically there are no signs and symptoms in the early stages of osteopenia and osteoporosis, once your bones have been weakened by, you might have some signs and symptoms that can indicate bone loss:
Early stage osteoporosis signs and symptoms
- Receding gums. If your jaw is losing bone, your gums may move back (recede).
- Weaker grip strength. In one study researchers found that low handgrip strength was linked to low bone mineral density.
- Weak and brittle fingernails. Nail strength may also indicate the health of your bones. However, nails may be brittle also because of other reasons such as for example some artwork, swimming or gardening (2, 3).
Later-stage osteoporosis signs and symptoms
- Back pain, or neck pain. Osteoporosis may lead to compression fractures of the spine which can be from minor to extremely painful, as the collapsed vertebrae may pinch the nerves that radiate out from the spinal cord.
- A stooped posture or compression fracture. The compression of the small bones that form the spine (vertebrae) may also cause a small curving of the upper back.
- A stooped back, also known as kyphosis can cause back and neck pain and even affect breathing due to extra pressure on the airway and limited expansion of your lungs.
- Loss of height over time. This is one of the most visible symptoms of osteoporosis, because these compression fractures in the spine may also lead to a loss of height.
- A bone that breaks extremely easily. Fractures may happen even with a minor movement or fall (1, 2, 3).
Osteopenia Causes, Risk Factors and Risk Groups
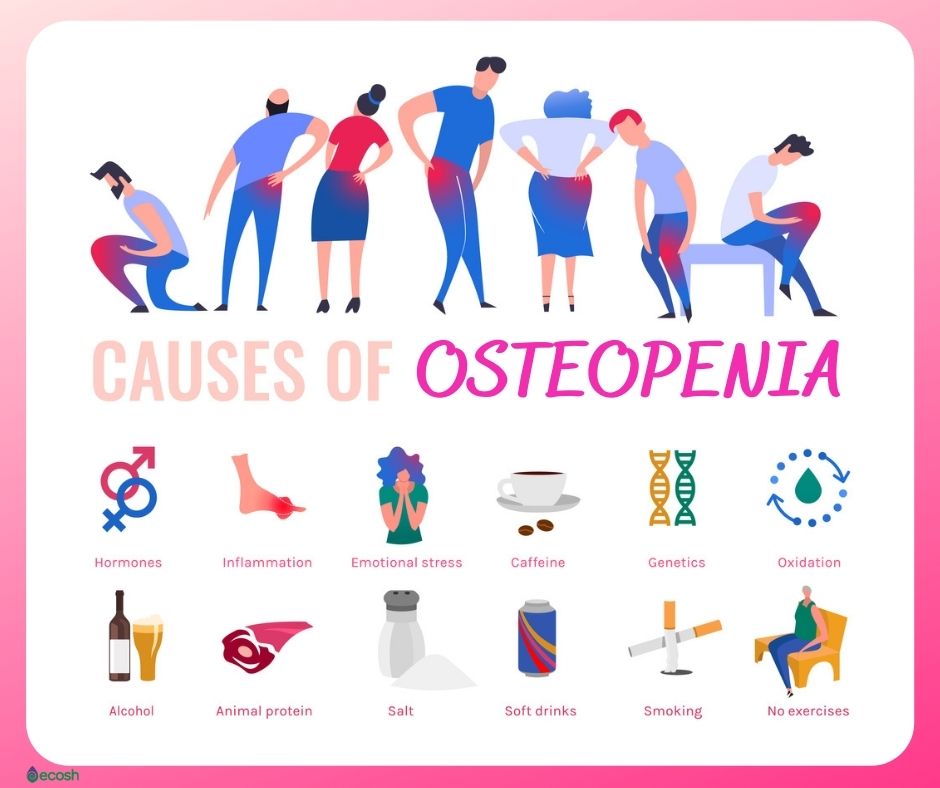
It’s totally normal that bones get weaker as people get older. However, some health conditions, medications and lifestyle choices may accelerate the process (2).
Many factors may increase the risk of developing osteopenia:
- A family history of low bone density (BMD)
- Older age than 50
- Poor diet, and low levels of calcium and vitamin D
- Being Caucasian or Asian. About a third of white and Asian men over age 50 have low bone density. Among Hispanics (23%) and blacks (19%) the prevalence is lower.
- Eating disorders such as anorexia or bulimia
- Not enough regular physical activity (especially strength-training exercise) or long periods of inactivity (such as long-term bed rest)
- Low body mass index (BMI) for example 19 or less
- Excess alcohol and caffeine drinking, and smoking
- In women, low oestrogen levels after the menopause may lead to a rapid decrease in bone density. Women are at even higher risk of developing osteoporosis if they have:
- menopause before age 45
- removal of the ovaries before age 45
- In men, low levels of testosterone
- Certain medical conditions such as:
- inflammatory conditions (for example rheumatoid arthritis, lupus, or Crohn’s)
- hormone-related conditions and a disorders of the hormone-producing glands
- malabsorption because of health conditions such as for example celiac sprue
- hyperthyroidism
- hyperparathyroidism
- Cushing syndrome
- Taking some medications such as for example:
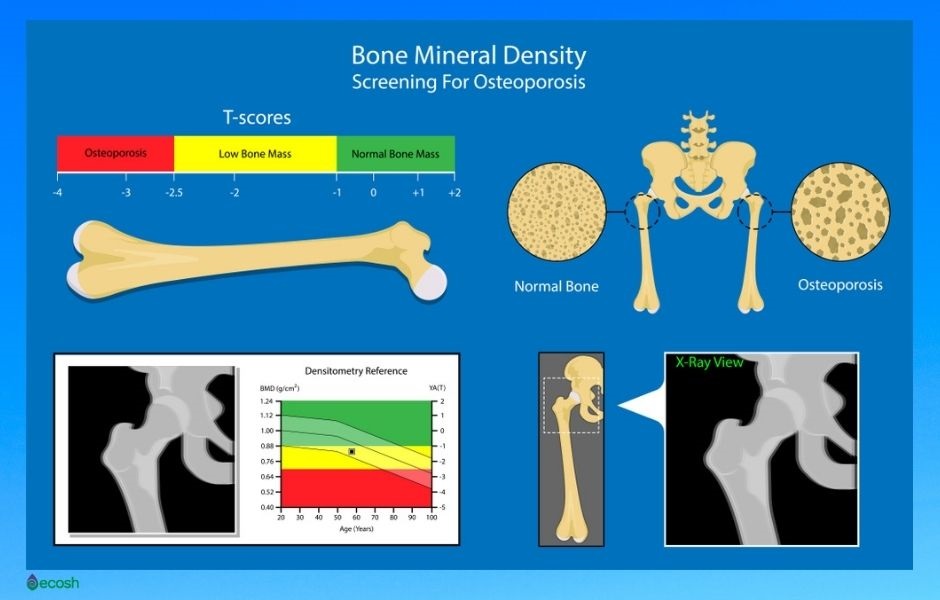
Diagnosing Osteopenia and Osteoporosis – The Bone Density Test
Although there are also other methods, the main way to determine your bone density is to have a dual-energy x-ray absorptiometry (also called DXA or DEXA) test that is painless, noninvasive and measures the mineral content of bone. In short, the test shows which category – normal, osteopenia, or osteoporosis – a person falls into compared to a normal 30 year old person of the same sex and age (21, 22, 26, 28).
How to read the results of the bone density test
T-score
- -1 and above: Normal
- -1 to -2.5: Low bone mass, a sign of osteopenia
- -2.5 and below: You likely have osteoporosis (28).

Osteopenia Prevention – 8 Tips to Prevent Osteopenia
The best way to hold back osteopenia is to avoid the lifestyle that causes it, and maintain a healthy diet (with adequate amounts of vitamin D and calcium). That is vital for individuals of all ages, but especially important if you’re younger than age 35, as then you can still build bone.
However, sometimes it might be not possible to prevent osteopenia and the best you can do is to prevent it from developing into osteoporosis (22, 24). Here are some tips to keep your bones in good shape.
1. Exercising regularly, as regular exercise is vital for healthy bones
- Aerobic activities. Individuals aged 19 to 64 should do at least 2 hours and 30 minutes of moderate-intensity aerobic activity each week. For example cycling, fast walking, or swimming
- Weight-bearing exercises (also resistance exercise) where your feet and legs support your weight are particularly important for improving bone density and helping to prevent osteoporosis. Individuals over the age of 60 may also benefit from regular weight-bearing exercise. Weight-bearing exercises include for example brisk walking, keep-fit classes or tennis, but not swimming and cycling.
- High-impact weight-bearing exercises are extremely vital for strengthening your muscles, joints and ligaments. These exercises are for example aerobics, dancing, hiking, running, skipping, stair climbing and even jumping up and down on the spot.
- Muscle-strengthening activities. Individuals aged 19 to 64 should also do muscle-strengthening activities on 2 or more days a week by working all the major muscle groups, including the legs, hips, back, abdomen, chest, arms and shoulders.
- Resistance exercises. These exercises use muscle strength and boosts bone strength, as the action of the tendons pulling on the bones. Examples include press-ups, weightlifting or using weight equipment at a gym (1, 4, 22).

2. Calcium
Calcium is important for maintaining strong bones. According to Mayo Clinic, all adults between the ages of 18 and 50 need 1,000 milligrams of calcium a day, which you should be able to get from your daily diet. However, this daily amount increases to 1,200 milligrams when women turn 50 and men turn 70 (1). You can use the calcium calculator on the IOS (International Osteoporosis Foundation) site to see if your diet includes an adequate amount of the vital nutrients for your bones.
Calcium-rich foods include for example:
- Leafy green vegetables like for example turnips, spinach, and kale
- Dried fruit
- Tofu
- Yoghurt
- Cheese
- Milk
- Canned salmon or sardines with bones
- Sardines
- Fortified cereals
- Fortified orange juice
- Soybeans and fortified soymilk
- Enriched breads, grains, and waffles (1, 4, 7).
3. Magnesium
Even though the evidence is still fragmented, most of the data accessible point to Magnesium as a benefactor element to bone health. Magnesium deficiency is linked to osteoporosis, as it acts on crystal formation and on bone cells. Magnesium also impacts on the secretion and the activity of parathyroid hormone and promotes low grade inflammation.
Therefore, optimizing magnesium intake might represent an effective and low-cost preventive measure against osteoporosis in individuals with magnesium deficiency.
However, too much Magnesium seems to have harmful effects on the bone, so be sure about your recommended daily allowance before taking any dietary supplements (16).
Magnesium rich foods are for example:
- Fish like Chinook salmon, halibut, mackerel or pollock
- Spinach
- Swiss chard
- Edamame
- Tamarind
- Potato with skin
- Okra
- Black-eyed peas (cooked)
- Tempeh (cooked)
- Soy nuts
- Cooked beans (black, lima, navy, pinto, chickpeas)
- Tofu
- Almonds
- Cashews
- Flaxseed
- Peanut butter
- Mineral or mineralized water (17).

4. Vitamin D
Vitamin D is vital for healthy bones because together with calcium, optimal amounts of vitamin D may help support bone health, prevent osteomalacia (softening of the bones due to a disorder of bone mineralization) and osteoporosis (thinning of the bone) ( 8, 9, 10, 11, 12, 13, 14).
According to Mayo Clinic, to get enough vitamin D to maintain bone health, it’s suggested that all adults (aged 51 to 70) get 600 IU daily, and older adults (after the age 70) 800 IU a day through food or dietary supplements.
Individuals who do not consume enough vitamin D-rich foods or especially people with limited sun exposure might need a dietary supplement (1, 4). See the recommended daily allowances here.
Vitamin D-rich foods include:
- Cod liver oil: 34.0 mcg (1,360 IU)/1 tbsp – 170% DV
- Trout (rainbow), farmed, cooked: 16.2 mcg (645 IU)/3oz – 81% DV
- Salmon (sockeye), cooked: 14.2 mcg (570 IU)/3 oz – 71% DV
- Mushrooms, white, raw, sliced, exposed to UV light: 9.2 mcg (366 IU)/ ½ cup – 46% DV
- Milk, 2% milkfat, vitamin D fortified: 2.9 mcg (120 IU)/1 cup – 15% DV
- Soy, almond, and oat milks, vitamin D fortified, various brands: 2.5-3.6 mcg (100-144 IU)/1 cup – 13-18% DV
- Ready-to-eat cereal, fortified with vitamin D: 2.0 mcg (80 IU)/1 serving – 10% DV
- Sardines (Atlantic), canned in oil, drained: 1.2 mcg (46 IU)/2 sardines – 6% DV
- Egg, scrambled**: 1.1 mcg (44 IU)/1 large – 6% DV
- Liver, beef, braised: 1.0 mcg (42 IU)/3 oz – 5% DV
- Tuna fish (light), canned in water, drained: 1.0 mcg (40 IU)/ 3 oz – 5% DV
- Cheese, cheddar: 0.3 mcg (12 IU)/1 oz – 2% DV
- Mushrooms, portabella, raw, diced: 0.1 mcg (4 IU)/½ cup – 1% DV
- Chicken breast, roasted: 0.1 mcg (4 IU)/3 oz 1% DV
- Beef, ground, 90% lean, broiled: 0 mcg (1.7 IU)/3 oz – 0% DV (15).
- mcg (μg) – Micrograms per serving
- IU – International Units per serving
- DV – Percent Daily Value
- oz – ounces
- ** Only egg yolk contains vitamin D
- 1 mcg (μg) of vitamin D is equivalent to 40 IU

5. Vitamin K-2
There is some limited evidence that also certain other supplements, such as vitamin K-2 and soy, may help lower fracture risk in case osteoporosis. However more studies are needed to prove these health benefits and determine risks (27).
6. Normal weight
Low body weight, especially BMI (Body Mass Index) 19 or less, has been associated with an increased risk of osteoporosis, as it raises the chance of bone loss and fractures. However, excess weight isn’t beneficial also, as it’s known now to increase the risk of fractures in your arm and wrist. Therefore, maintaining a suitable balance in your body weight is beneficial for your bones and for your overall health as a whole (1).
7. Quit smoking and drink in moderation
- Consistent drinking of more than two alcoholic beverages a day may increase your risk of osteoporosis. Therefore, the NHS recommends not to drink more than 14 units of alcohol a week. Also, it’s vital to avoid binge drinking (1, 4).
- The exact reason why tobacco plays a role in osteoporosis isn’t totally clear yet, however, smoking is associated with an increased risk of weak bones and osteoporosis (1, 4).

8. Smile to sun
Vitamin D (D3 – cholecalciferol) is produced in the skin from 7-dehydrocholesterol by the sun (or ultraviolet light UV) with an UV index of 3 or more. Therefore, to maintain healthy vitamin D levels in your body, which helps your body absorb calcium, you should aim to get 10–30 minutes of midday sunlight, several times per week.
However, people with darker skin may need a little more than this (4, 18, 19). As nowadays people stay and work more indoors, the vitamin D deficiency is very common. Therefore, to obtain sufficient amounts of vitamin D you can eat more vitamin D rich foods or take vitamin D supplements, as low vitamin D levels might contribute to osteoporosis.
However, do not start to self medicate and consult your doctor if you suspect osteopenia or osteoporosis. Your doctor will then make the necessary tests such as for example bone density tests, and suggests the treatment.
Osteopenia Treatment
As osteopenia treatment depends individually, the first step is to find out if the person is at a high risk for fracture. In this case, doctors suggest certain bone health medications to build the skeleton back up as much as possible and to prevent bone breakdown.
However, for all people with osteopenia, regular weight-bearing exercise, eating foods rich in calcium and vitamin D is crucial. As vitamin D is hard to get from food, a vitamin D supplement may help (21, 23).
NB! The information provided here is for informational purposes only, so do not consider it as health care or medical diagnosis and treatment. Do not consider this information as a guarantee of the results you want to achieve. In addition, this information here is not intended to replace the advice of your physician or other healthcare professional.
Even more, you should not use it to diagnose or treat a health problem. Before changing or discontinuing your existing medication, treatment, or care, or taking any dietary supplements, be sure to consult with your healthcare professional or doctor before starting any diet or program, or if you suspect you may have a medical condition.
Compiled by Maria-Helena Loik
Pictures: Pexels.com, Pixabay.com, Shutterstock.com
Sources:
- Osteoporosis – Symptoms and causes – Mayo Clinic
- Osteoporosis Symptoms: Early and Late Stages (healthline.com)
- Low Grip Strength is a Strong Risk Factor of Osteoporosis in Postmenopausal Women – PubMed (nih.gov)
- Osteoporosis – NHS (www.nhs.uk)
- The effect of vitamin D on bone and osteoporosis – PubMed (nih.gov)
- Calcium, vitamin D, and fractures (oh my!) – Harvard Health Blog – Harvard Health Publishing
- Top 10 Calcium-Rich Foods (webmd.com)
- https://en.wikipedia.org/wiki/Vitamin_D
- https://www.nhs.uk/conditions/vitamins-and-minerals/vitamin-d/#:~:text=Vitamin%20D%20helps%20regulate%20the,condition%20called%20osteomalacia%20in%20adults.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3221132/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2621390/
- https://pubmed.ncbi.nlm.nih.gov/31454046/
- https://pubmed.ncbi.nlm.nih.gov/31454046/
- pubmed.ncbi.nlm.nih.gov/31454046/
- https://ods.od.nih.gov/factsheets/VitaminD-HealthProfessional/
- Magnesium and Osteoporosis: Current State of Knowledge and Future Research Directions (nih.gov)
- The Best Foods That Are High in Magnesium (webmd.com)
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3356951/#:~:text=Vitamin%20D3%20(cholecalciferol)%20is,scientifically%20known%20as%2022%2Ddihydroergocalciferol.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3356951/#:~:text=Vitamin%20D3%20(cholecalciferol)%20is,scientifically%20known%20as%2022%2Ddihydroergocalciferol.
- Learn What Osteoporosis Is and What It’s Caused by (nof.org)
- Osteopenia: When you have weak bones, but not osteoporosis – Harvard Health
- Osteopenia: Treatment, Symptoms, Diet, and Diagnosis (healthline.com)
- What Is Osteopenia? Causes, Symptoms and Treatment (hss.edu)
- Does Osteopenia Hurt? Causes, Treatment & Diet (medicinenet.com)
- CALCIUM – Calcium Calculator | International Osteoporosis Foundation
- Bone density test – Mayo Clinic
- Osteoporosis – Diagnosis and treatment – Mayo Clinic
- How osteoporosis is diagnosed – Mayo Clinic