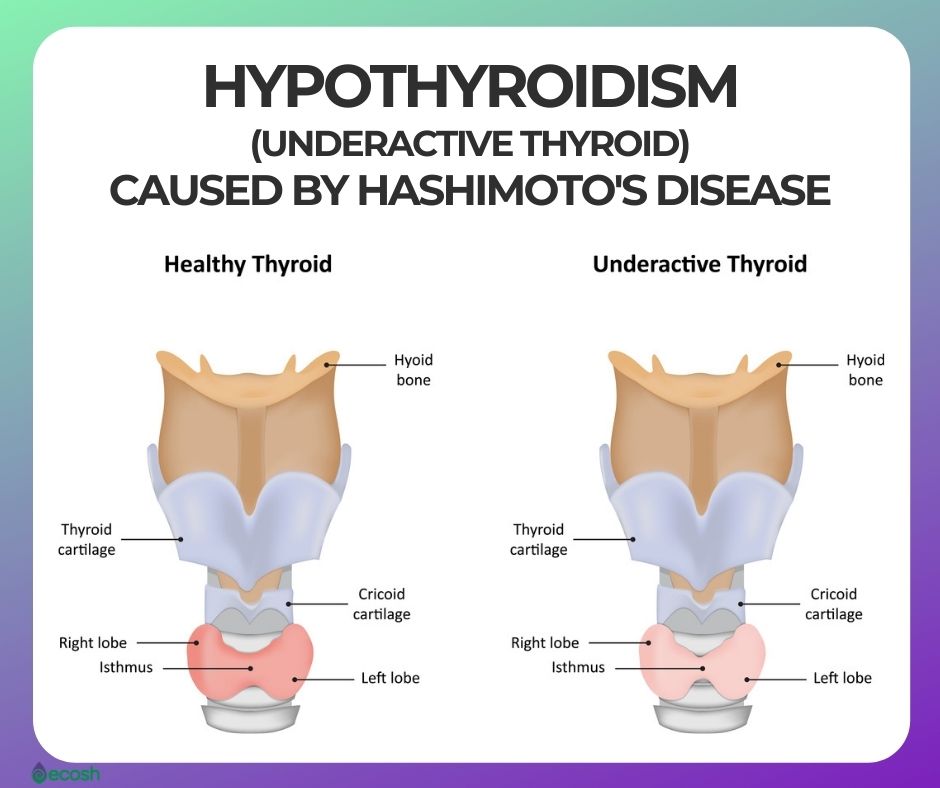
Hashimoto’s disease (also called Hashimoto’s thyroiditis, chronic lymphocytic thyroiditis, or autoimmune thyroiditis) is an autoimmune disorder in which the immune system attacks your thyroid, and causes thyroid damage. Due to this damage, the thyroid can’t make enough thyroid hormones, and the production of thyroid hormones slows down to a deficiency.
The thyroid, which is a butterfly-shaped gland that`s located low on the front of the neck below your Adam’s apple, wrapped around the windpipe (trachea), controls your metabolism with a few specific hormones which are created by the thyroid and tell your body’s cells how much energy to use.
Therefore, thyroid hormones affect just about every organ in your body, even the way your heart beats.
Inflammation from Hashimoto’s disease frequently leads to an underactive thyroid. Therefore, Hashimoto’s disease is the most common cause of hypothyroidism (underactive thyroid), and affects about 5 people out of 100 in the United States. Symptoms of Hashimoto’s disease commonly include fatigue, swelling of the thyroid (goiter), weight gain, hair loss and sensitivity to cold. It typically affects middle-aged women but can also happen in children, and in men and women of any age.
Treatment for Hashimoto’s disease with thyroid hormone replacement is usually simple and effective. In addition, you may find some help in alternative medicine, Hashimoto’s diet and certain supplements (1, 2).
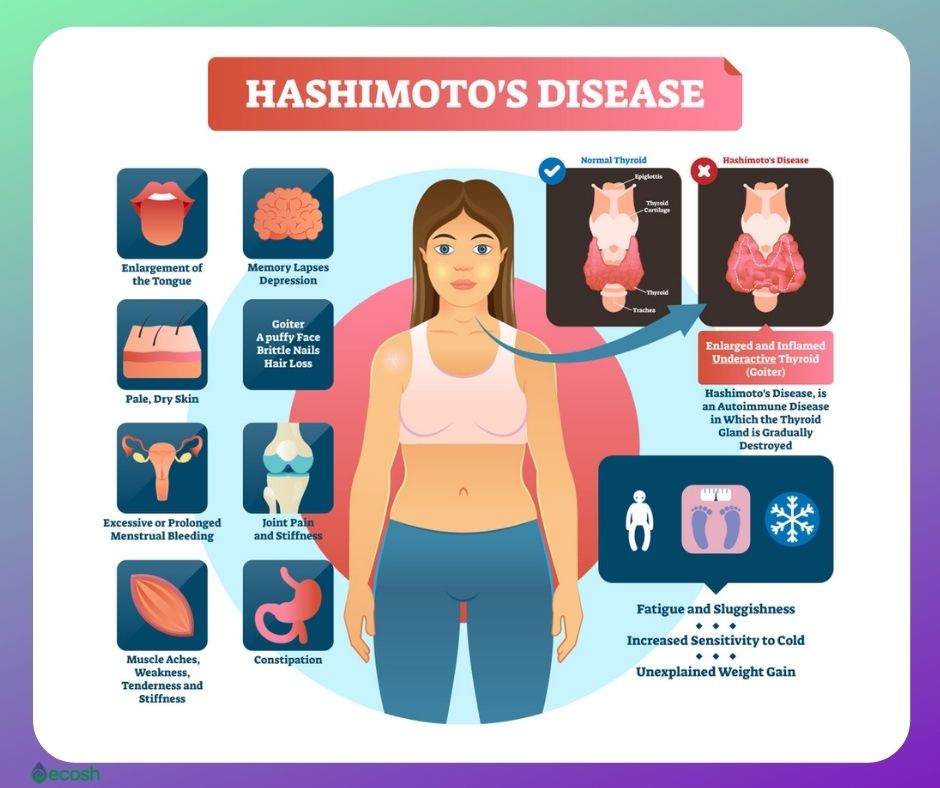
Hashimoto’s Disease Signs and Symptoms
Hashimoto’s disease generally progresses slowly over years and causes chronic thyroid damage which leads to a fall in thyroid hormone levels. However, for many people, Hashimoto’s disease may not cause any symptoms at first.
When Hashimoto’s disease slowly progresses, the thyroid commonly gets bigger (goiter) and may cause the front of the neck to look swollen. This may create a feeling of fullness in your throat, though it is usually not painful.
The signs and symptoms of Hashimoto’s thyroiditis (mainly those of an underactive thyroid gland (hypothyroidism)) include:
- Tiredness
- Fatigue and sluggishness
- Being sensitive to cold
- Constipation
- Dry and pale skin
- A puffy face
- Brittle nails
- Dry and thinning hair
- Hair loss
- Enlargement of the tongue
- Unexplained weight gain
- Muscle aches, tenderness and stiffness
- Joint pain and stiffness
- Muscle weakness
- Heavy or irregular menstrual periods
- Problems becoming pregnant
- Depression
- Memory problems and lapses
- A slowed heart rate
- Increased sensitivity to cold (1, 2, 3).
Hashimoto’s Disease Causes
Hashimoto’s disease is an autoimmune disorder in which your immune system makes antibodies that attack the thyroid gland. Researchers don’t know what causes your immune system to attack your thyroid gland.
However, some scientists think the disorder probably results from the virus, bacterium, or an outside trigger, while others believe a genetic defect may be involved (3).
Hashimoto’s Disease Risk Groups
- Gender. Hashimoto’s disease occurs about 8 times more frequently among women than men.
- Age. Although the disease can occur at any age, more commonly it appears during middle age – between ages 40 and 60.
- Genetics. You’re at greater risk for developing Hashimoto’s disease if other family members have thyroid or other autoimmune diseases.
- Radiation exposure. Individuals who are exposed to excessive levels of environmental radiation are more vulnerable to Hashimoto’s disease.
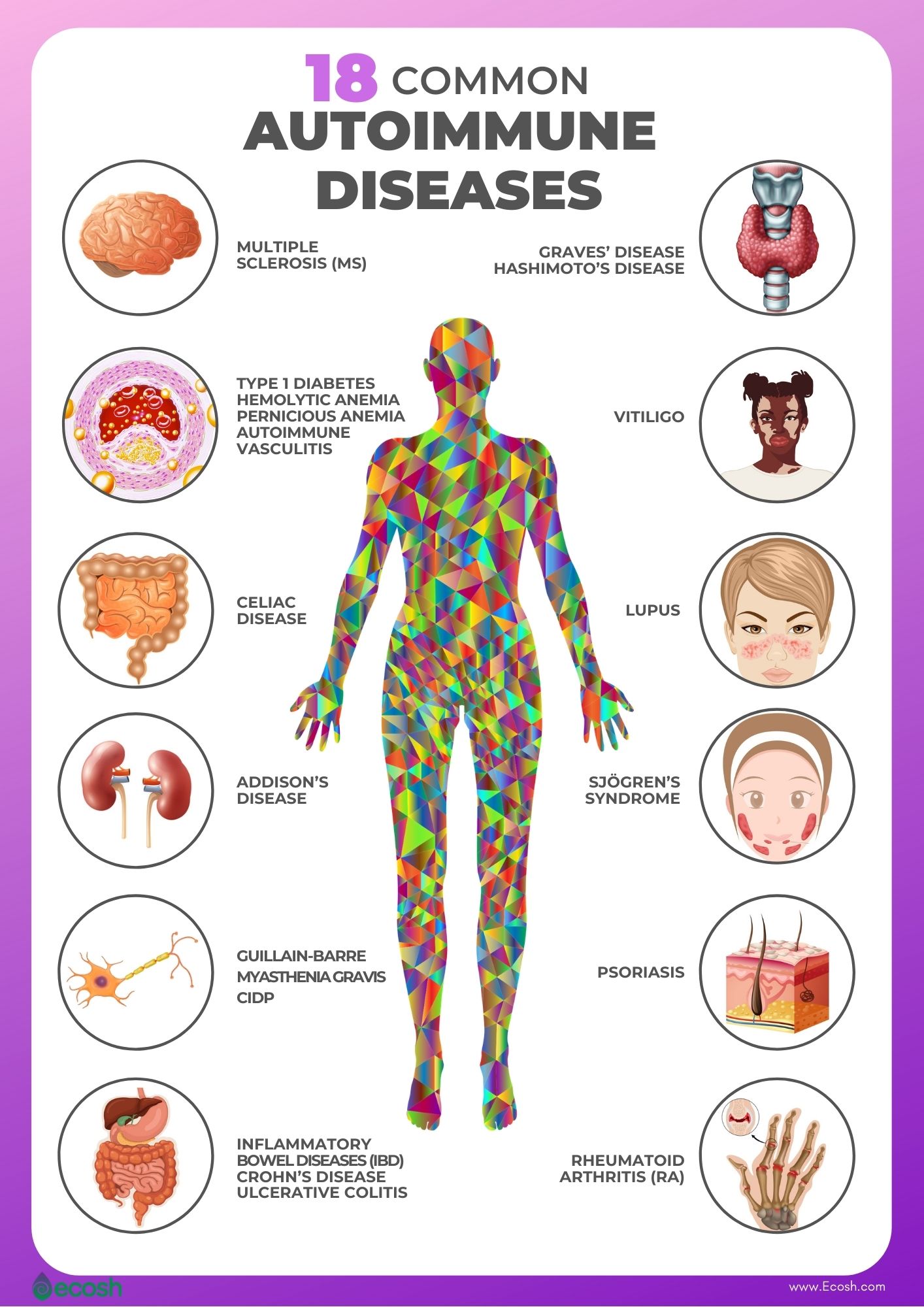
- Other autoimmune diseases. People with other autoimmune disorders are at higher risk to develop Hashimoto’s disease. Autoimmune diseases associated to Hashimoto’s disease include:
- Addison’s disease
- Autoimmune hepatitis
- Celiac disease
- Lupus
- Pernicious anemia (vitamin B12 deficiency)
- Rheumatoid arthritis
- Sjögren’s syndrome
- Type 1 diabetes
- Vitiligo (1, 3).
Hashimoto’s Disease Complications
Without treatment, hypothyroidism (underactive thyroid gland), caused by Hashimoto’s disease, may lead to several health issues:
Heart problems. Low levels of thyroid hormones are associated with high levels of bad cholesterol (low-density lipoprotein (LDL) cholesterol) that can lead to heart disease. Therefore, without treatment, hypothyroidism may cause an enlarged heart and, perhaps, heart failure.
Goiter. In order to release more hormones, the continuous stimulation of your thyroid may cause the gland to become enlarged (a goiter). Ordinarily, it is not uncomfortable, but it can influence your appearance and may impede swallowing or breathing.
Mental health issues and depression. In Hashimoto’s disease, depression may develop early and become more serious over time. It may also cause slowed mental functioning.
Decreased sexual desire (libido). This disease may also lead to reduced sexual desire in men as well as in women.
Seizures. In case of very severe hypothyroidism that hasn’t been diagnosed or treated, your risk of developing low serum sodium goes up and this could lead to seizures.
Peripheral neuropathy.
Myxedema (miks-uh-DEE-muh). In rare cases, severe, untreated hypothyroidism may cause an extreme condition called myxedema coma, in which the body’s functions slow to the point that it becomes life-threatening. Its signs include drowsiness, profound lethargy and unconsciousness. This condition may be triggered by sedatives, exposure to cold, infection or other stress on your body. Myxedema coma requires urgent emergency medical treatment.
Infertility.
Birth defects. If left untreated, hypothyroidism may cause serious problems for the mother as well as for the baby. There may be a link between hypothyroid pregnancies and birth defects, such as a cleft palate, and heart, brain and kidney problems in infants. Also, babies born to women with untreated hypothyroidism due to Hashimoto’s disease are more prone to intellectual and developmental problems. However, medications for thyroid can help prevent these issues and are usually safe to take during pregnancy. In addition, during pregnancy, many women who take thyroid hormone medication, may need a higher dose. Therefore, consult your doctor right away if you find out that you’re pregnant. If you’re planning to get pregnant or if you’re in early pregnancy, be sure to have your thyroid level checked (1, 2).

Hashimoto’s Disease Treatment – Conventional Medicine, Alternative Treatment, Supplements and Hashimoto’s Disease Diet
Conventional Medicine
Treatment for Hashimoto’s disease usually depends on whether your thyroid is damaged enough to cause hypothyroidism. If you don’t have hypothyroidism, and your thyroid is functioning normally, your doctor may suggest to simply monitor you to see if your disease gets worse. However, if you need medication, chances are you’ll need it for the rest of your life.
In this case, never skip doses, stop taking your medicine, or change the brand without talking with your doctor first, as signs and symptoms will gradually return.
Synthetic hormones. The most common hypothyroidism treatment is replacing the hormone that your own thyroid can no longer produce. This usually involves daily use of the synthetic thyroid hormone levothyroxine (Levoxyl, Synthroid, others) that is identical to a hormone the thyroid normally makes, restores sufficient hormone levels in your body, and reverses all the symptoms of hypothyroidism.
Monitoring. To determine the right dosage of levothyroxine initially, your doctor will give you a blood test about 6 to 8 weeks after you begin taking thyroid hormone and adjust your dose if needed. Once the dose that normalizes your thyroid tests is determined, your doctor is likely to check your TSH level about once a year as the dosage you need may change. When used in the appropriate dose, levothyroxine does not cause practically any side effects. However, excessive amounts of thyroid hormone and overtreatment with levothyroxine may include health risks such as:
- Acceleration of bone loss, which may make osteoporosis worse or add to your risk of this disease.
- Heart rhythm disorders (arrhythmias).
Reaction of other substances. Some supplements, medications and certain foods may influence your ability to absorb levothyroxine. However, taking levothyroxine 4 hours before or after other medications may resolve this issue. Consult your doctor if you:
- Eat large amounts of soy products or a high-fiber diet.
- Take supplements such as iron supplements (including multivitamins that contain iron), and calcium supplements.
- Take medications such as Cholestyramine (a medication used to lower blood cholesterol levels), Sucralfate (an ulcer medication), or medications that contain Aluminum hydroxide (found in some antacids).
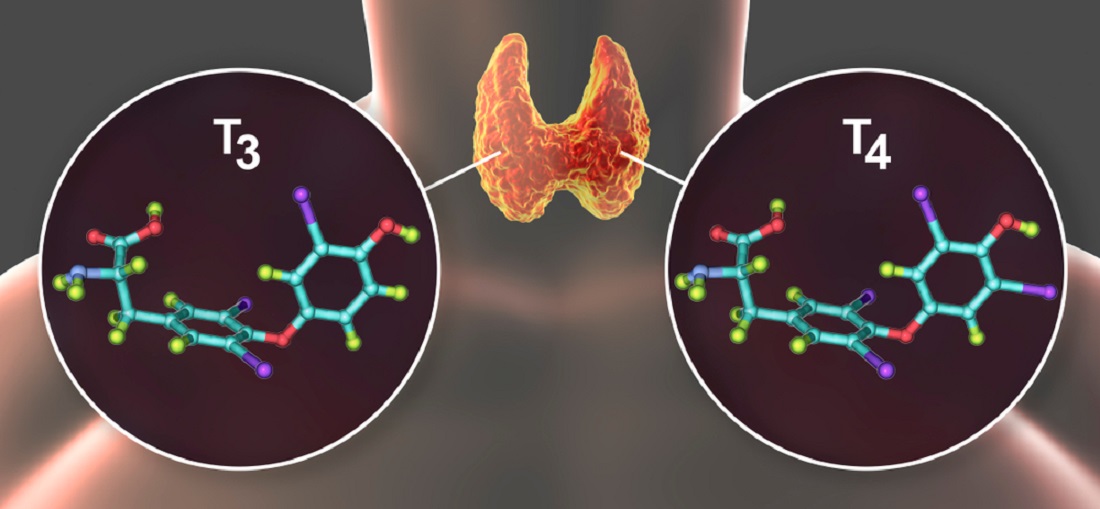
Combination of hormones. In your body, T-4 (levothyroxine is the synthetic form of the natural thyroid hormone T-4) is converted into T-3. Research about whether adjusting standard hypothyroidism treatment to replace some T-4 with small amounts of T-3 (T-3 can be given alone as liothyronine (Cytomel) or in combination with T-4) may offer benefit is still ongoing. However, for those who haven’t gotten enough relief from T-4 alone, adding liothyronine to standard levothyroxine treatment for a 3 to 6 month trial is a long enough period to see if the combination helps you. Taking a combination T-4 and T-3 ends up making more than normal levels of T-3, particularly soon after the medication is taken. This can cause a fast heart rate, anxiety and trouble sleeping (3).
Alternative Treatment, Supplements and Hashimoto’s Disease Diet
Natural extracts containing thyroid hormone such as desiccated thyroid extract. Even though most healthcare providers suggest synthetic thyroxine, natural extracts containing thyroid hormone derived from the thyroid glands of pigs are also available. These products such as for example Armour Thyroid — contain both levothyroxine and triiodothyronine (T-3). However, these extracts are available by prescription only, so do not confuse these with the glandular concentrates sold in natural foods stores. Moreover, doctors have a number of concerns about such thyroid hormone extracts such as Armour Thyroid, including:
Iodine balance. Thyroid uses iodine to produce hormones. An iodine deficiency is a very common issue among several million people around the world. However, people with Hashimoto’s disease or other types of autoimmune thyroid disorders may be sensitive to harmful side effects from iodine, and taking in too much iodine can also cause or worsen hypothyroidism. Therefore, the most important is the iodine balance. Kelp, dulse and other types of seaweed contain a lot of iodine. In addition, cough syrup and multivitamins may also contain iodine. In American Thyroid Association page you will find low iodine diet tips to follow. During pregnancy, women need a little more iodine, as the baby gets iodine from the mother’s diet. However, excessive iodine can also cause problems, such as goiter in the baby. If you are pregnant, talk with your doctor about how much iodine you need Low in iodine foods and drinks include:
- non iodized salt
- egg whites
- vegetables (fresh or frozen), vegetable oils and fruits
- drinks such as tea, black coffee, soda, lemonade, fruit juices, beer and wine
- herbs and spices
- honey, sugar, jam, and jelly
- unsalted nuts and nut butter
- in addition, beef, chicken, turkey, veal, and lamb (moderate servings) (1, 6).

Hashimoto’s Diet. Research shows that not eating some foods, taking certain supplements, and making lifestyle changes may remarkably improve symptoms and quality of life among Hashimoto’s disease patients. In addition, these changes may help lessen inflammation in your body, slow or prevent thyroid damage caused by elevated thyroid antibodies, and control body weight, cholesterol levels, and blood sugar (7).
Gluten-free diet. According to studies, gluten-free diet may be beneficial for individuals with Hashimoto’s disease (or with other autoimmune diseases) even if they don’t have celiac disease (a treatable, gluten-induced disease that often occurs concurrently with other autoimmune diseases) (7, 8, 9). In gluten-free diet people avoid all wheat (pastas, breads), barley, rye products, and soy sauces that may also contain gluten.
The Autoimmune Protocol (AIP) Diet. This certain diet is designed for individuals with autoimmune diseases. AIP Diet eliminates potentially harmful foods such as added sugar, refined sugars, grains, dairy, nightshades, coffee, legumes, eggs, alcohol, nuts, seeds, oils, and food additives, but is rich in whole, nutrient-dense foods such as vegetables, fruits, proteins, healthy fats, and fiber-rich carbs. However, do not practice AIP Diet by yourself, as it should be prescribed and monitored by an experienced healthcare provider (7, 10).
Think about avoiding dairy. As lactose intolerance is very common among people with Hashimoto’s disease, cutting out dairy may aid digestive problems, as well as thyroid function and medication absorption. However, this strategy may not have benefits for everyone, as some individuals with Hashimoto’s disease tolerate dairy quite well (7, 11).
Anti-inflammatory and antioxidant rich foods. According to a study, individuals with Hashimoto’s disease under thyroxine replacement have higher markers of oxidative stress (a condition that causes chronic inflammation). Inflammation due to Hashimoto’s disease (chronic lymphocytic thyroiditis), often leads to an underactive thyroid gland (hypothyroidism). However, normal BMI, daily antioxidant rich fruit and vegetable consumption, all contribute in maintaining oxidative stress at low levels. Anti-inflammatory and antioxidant rich foods include foods such as tomatoes, olive oil, green leafy vegetables (like spinach, kale, and collards), nuts (like almonds and walnuts), fatty fish (like salmon, mackerel, tuna, and sardines), fruits and berries (like strawberries, blueberries, cherries, and oranges) (7, 12, 13, 14).
Low carbohydrate diet and avoiding goitrogenic foods. According to a study, a dietary plan based on the reduction of carbohydrate content and free of goitrogenic foods (goitrogens are substances found in soy products and cruciferous vegetables) may lead to a decreased body weight, as well as decreased fat mass and a significant drop of sentinel autoantibodies in Hashimoto’s thyroiditis (15). However, cooking cruciferous vegetables decreases their goitrogenic activity (7, 16).
Avoiding soy products. Although more research is needed, according to some evidence, soy may be harmful for thyroid function as well. Therefore, many people with Hashimoto’s choose to avoid soy products (7, 17, 18).
Supplements. As people with Hashimoto’s disease are more likely to be deficient in some nutrients, supplementing may be necessary, and certain supplements may help lessen inflammation and thyroid antibodies in people with this condition. However, taking high doses of iodine or supplements that contain iodine in the absence of an iodine deficiency may lead to adverse effects in those with Hashimoto’s. Therefore, consult your healthcare provider before taking any supplements (19, 20, 21). Supplements that might be beneficial for Hashimoto’s patients include:
Selenium. Although further studies are needed to confirm this benefit, selenium supplementation in patients with Hashimoto’s thyroiditis with known selenium deficiency may be useful, even for those who are already being treated with levothyroxine. Studies show that taking selenium may help reduce antithyroid peroxidase (TPO) antibodies and improve overall well-being in people with Hashimoto’s disease (22, 23).
Zinc. Scientific evidence shows that zinc plays a key role in the metabolism of thyroid hormones, specifically by regulating deiodinases enzymes activity, thyrotropin releasing hormone (TRH), and thyroid stimulating hormone (TSH) synthesis, as well as by adjusting the structures of vital transcription factors involved in the synthesis of thyroid hormones. Serum concentrations of zinc also seem to affect the levels of serum T3, T4 and TSH. Therefore, zinc is essential for thyroid function (24, 25).
Iron. Individuals with Hashimoto’s disease and hypothyroidism are more likely to develop anemia. Therefore, people with these conditions may also need iron supplements (26).
B complex vitamins. People with Hashimoto’s disease and underactive thyroid (hypothyroidism) often develop vitamin B12 deficiency. Therefore, taking a vitamin B-12 supplement may help you with the tiredness and repair some of the other damage hypothyroidism caused. As the disease also influences your vitamin B-1 levels, you can take vitamin B complex supplements or add more B vitamins to your diet. However, talk with your doctor about how much vitamin B-12 may be right for you.
(19, 27).Curcumin. According to animal and human studies this powerful anti-inflammatory and antioxidant compound may be beneficial in treatment of autoimmune diseases and inflammatory conditions in general (28, 29, 30).
Vitamin D. Several studies have observed a relationship between vitamin D deficiency and thyroid diseases. Therefore, supplementary treatment with vitamin D3 (cholecalciferol) seems to have beneficial effects on autoimmune thyroid disorders (AITD) (31, 32).
Magnesium. Severely low levels of magnesium are linked with higher thyroid antibodies, and an increased risk of Hashimoto’s disease. Therefore, improving magnesium level in your body, may improve symptoms in individuals with thyroid disease (33, 34).
Fish oil, alpha-lipoic acid, and N-acetyl cysteine. Some other supplements like fish oil, alpha-lipoic acid, and N-acetyl cysteine could be useful in case hypothyroidism is caused by Hashimoto’s disease. However more studies are needed to confirm the results (35, 36, 37).
NB! The information provided here is for informational purposes only, so do not consider it as health care or medical diagnosis and treatment. Do not consider this information as a guarantee of the results you want to achieve. In addition, this information is not intended to replace the advice of your physician or other healthcare professional.
Even more, you should not use it to diagnose or treat a health problem. Before changing or discontinuing your existing medication, treatment, or care, or taking any dietary supplements, be sure to consult with your healthcare professional or doctor before starting any diet or program, or if you suspect you may have a medical condition.
Compiled by Maria-Helena Loik
Pictures: Pexels.com, Pixabay.com, Shutterstock.com
Sources:
- Hashimoto’s Disease | NIDDK (nih.gov)
- Symptoms and Causes of Hashimoto`s disease – Mayo Clinic
- Hashimoto’s disease (nchmd.org)
- Desiccated thyroid extract vs Levothyroxine
- Desiccated thyroid extract – Wikipedia
- Diet for hyperthyroidism – (medicalnewstoday.com)
- Hashimoto Diet (healthline.com)
- Hashimoto thyroiditis (HT), the importance of iodine, selenium, vitamin D and gluten – (nih.gov)
- Coeliac disease and autoimmune disease – PubMed (nih.gov)
- Efficacy of the AIP Diet for Hashimoto’s Thyroiditis (nih.gov)
- Decrease in TSH levels after lactose restriction – PubMed (nih.gov)
- The effect of obesity and dietary habits on oxidative stress in Hashimoto’s thyroiditis (nih.gov)
- Hashimoto’s disease – Symptoms and causes – Mayo Clinic
- Foods that fight inflammation – Harvard Health
- Effects of low-carbohydrate diet therapy in autoimmune thyroiditis – (nih.gov)
- The role of micronutrients in thyroid dysfunction (nih.gov)
- Soy isoflavones inducing overt hypothyroidism – (nih.gov)
- Various Possible Toxicants Involved in Thyroid Dysfunction – (nih.gov)
- Vitamin B12 and Vitamin D Levels in Autoimmune Hypothyroidism – Karger Publishers
- Effects of Increased Iodine Intake on Thyroid Disorders (nih.gov)
- Iodine-induced thyroid dysfunction (nih.gov)
- Selenium in Immune Mediated Thyroid Disorders (nih.gov)
- Selenium in the treatment of Hashimoto’s – PubMed (nih.gov)
- Effects of Zinc and Selenium on Thyroid Function – PubMed (nih.gov)
- The Role of Zinc in Thyroid Hormones Metabolism – PubMed (nih.gov)
- Thyroid Function and Anemia – (nih.gov)
- Vitamin B12 deficiency common in primary hypothyroidism – PubMed (nih.gov)
- Curcumin in Autoimmune and Rheumatic Diseases – PubMed (nih.gov)
- Curcumin, Inflammation, and Chronic Diseases: How Are They Linked? (nih.gov)
- Turmeric use is associated with reduced goitrogenesis – (nih.gov)
- The association between severity of vitamin D deficiency and Hashimoto’s thyroiditis – PubMed (nih.gov)
- Effects of Vitamin D in Thyroid Diseases (nih.gov)
- Severely low serum magnesium is associated with increased risks of hypothyroidism: (nih.gov)
- Magnesium deficiency due to physical and psychological stressors (nih.gov)
- Alpha-lipoic acid improves endothelial dysfunction – PubMed (nih.gov)
- The effect of omega-3 on cognition – PubMed (nih.gov)
- N-Acetylcysteine and 15 Deoxy-Δ12,14-Prostaglandin J2 Exert a Protective Effect Against Autoimmune Thyroid Destruction (nih.gov)


