Sleep disorders are a set of conditions that change the way you sleep and influence the ability to sleep well on a regular basis. A sleep disorder can greatly affect your quality of life, performance at work, weight, energy, mood, concentration, safety, cause problems in relationships, and increase your likelihood of developing other health problems when left untreated.
Therefore, it’s important to receive a diagnosis and treatment right away if you suspect you might have some type of sleep disorder.
According to a study, more than a third of American adults are not getting enough sleep on a regular basis, so you might say that unfortunately, sleep disorders have become increasingly common (8).
As there are many types of sleep disorders with different causes and symptoms, these disorders are often grouped into categories that explain how they affect you, why they happen and what is the best treatment. Here is the full and profound list of most common sleep disorders.
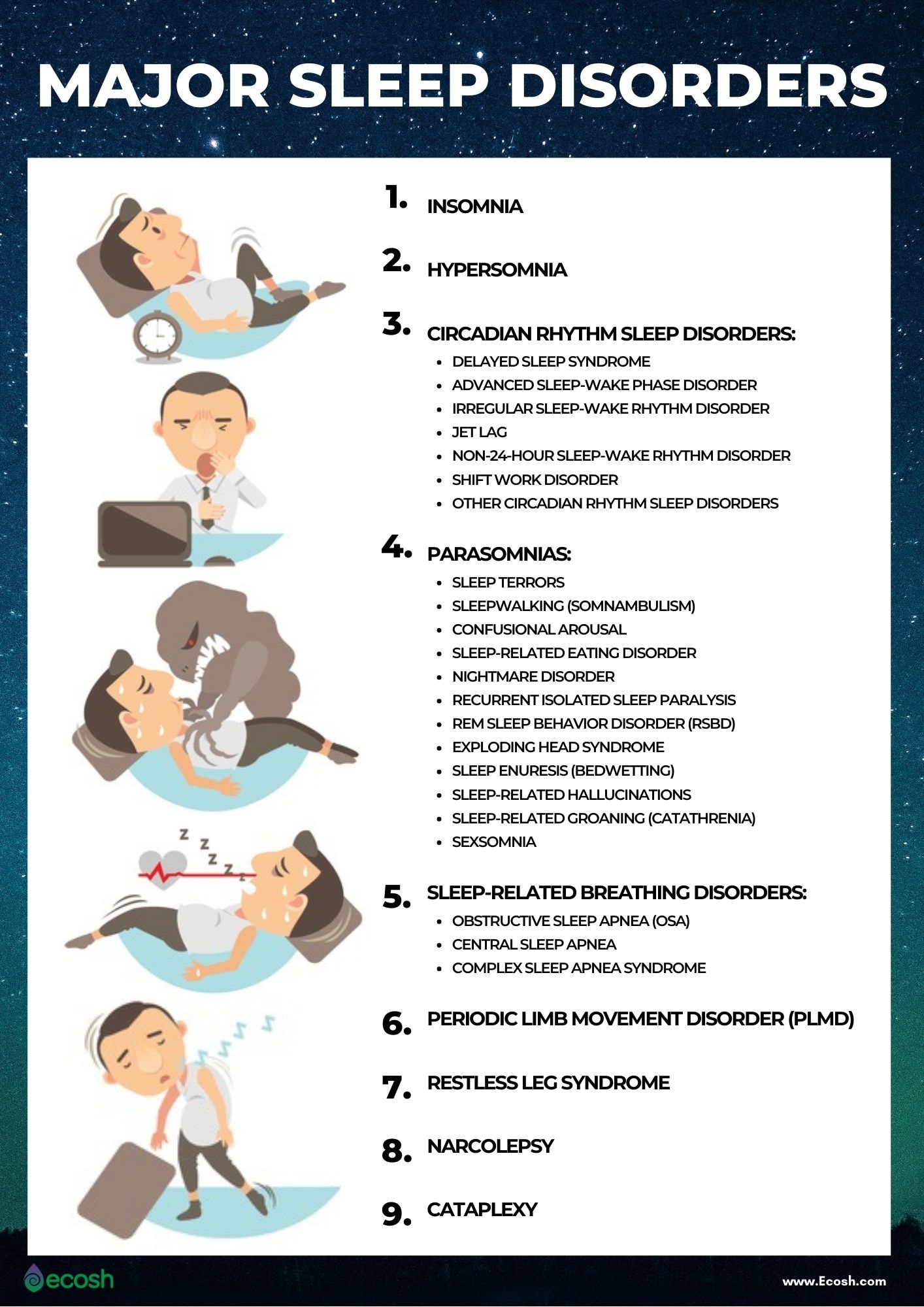
What are The Major Sleep Disorders? The Full List of Most Common Sleep Disorders
Some sleep disorders may be caused by health problems (sleep disorder can be a symptom of another mental or medical health condition), while other sleep problems can be caused by too much stress or hectic schedules. Sleeping problems caused by other health conditions may eventually go away once treatment is obtained for the underlying cause.
Some of the the signs of sleep disorders include excessive daytime sleepiness, irregular breathing or increased movement during sleep. While other symptoms include an irregular sleep and wake cycle and difficulty falling asleep.
1. Insomnia
Insomnia is the most common sleep disorder in which a person has trouble falling asleep, sleeping without constantly waking up, or waking up too early in the morning. In case of insomnia, you may find help in changing sleep habits, practicing good sleep hygiene, as well as certain supplements that help relax and promote sleep such as magnesium and good night sleep complex. Read more about the causes, risk factors and insomnia natural treatment here.
Main causes that may lead to insomnia include:
- Stress associated with major life events.
- Environment, such as noise or temperature.
- Irregular bedtime and changes in your usual sleep schedule.
- Blue light
- Mental health problems, as well as depression and anxiety.
- Medicines for colds, allergies, depression, high blood pressure and asthma.
- Nocturnal pain or discomfort.
- Consumption of stimulants like caffeine, tobacco or alcohol.
- Hyperthyroidism and other endocrine problems.
- Diseases such as asthma, arthritis, digestive problems, nerve diseases, cancer or heartburn.
- Other sleep disorders such as sleep apnea or restless legs syndrome (1).
2. Hypersomnia or Also Called Excessive Daytime Sleepiness (EDS)
The main signs of hypersomnia are excessive daytime sleepiness with sleep attacks or prolonged sleep. Excessive sleepiness during the day may occur even after long stretches of sleep. Hypersomnia can be caused by wide range of psychological and medical conditions, such as:
- Hypothyroidism
- Diabetes
- Chronic pain
- Depression
- Anxiety
- In addition, certain other sleep disorders like sleep apnea and periodic limb movement disorder (1).

3. Circadian Rhythm Sleep Disorder
Circadian rhythm sleep-wake disorder is explained as the lack of synchronism between a person’s individual sleep-wake cycle and the desired sleep-wake cycle, depending on environmental conditions. This sleep disorder often results in hypersomnia or insomnia.
Types of Circadian Rhythm Sleep Disorders include:
1. Delayed sleep syndrome or also called delayed sleep phase syndrome (DSPS)
While most people fall asleep in the evening between 10 and 12, in the case of delayed syndrome, sleep arrives 2-4 hours later than usual.
2. Advanced sleep-wake phase disorder
Sleep arrives a few hours (up more than two hours) earlier than usual or the desired times. This sleep-wake phase disorder should not cause significant problems in regulating work and rest time.
3. Irregular sleep-wake rhythm disorder
In case this disorder people have inconsistent sleep patterns without a stable rhythm or and day-night cycles. For example, sleep arrives every day, 1 hour later than the day before. The sleep cycle of this disorder usually yields periods of sleep that last four hours or less. As a result, people often nap throughout the day.
Irregular sleep rhythm can cause very significant stress, both to the person himself or herself and to others with whom he or she has family or work relationships. People with irregular sleep-wake rhythm disorder often also suffer from some neurodegenerative or neurodevelopmental disorder, such as Parkinson’s disease, Alzheimer’s disease, Huntington’s Disease, or developmental disabilities (in children).
4. Jet lag
Most people come up against jet lag after flights that pass over numerous time zones. The condition, in which people experience temporary sleep disturbances and daytime fatigue, represents a transition period during which a person’s internal clock needs to synchronize with local time. Jet lag symptoms commonly start one to two days after the flight and may continue for up to a week or two.
5. Non-24-hour sleep-wake rhythm disorder, also called free-running disorder
This disorder happens when the internal clock does not reset every 24 hours, and mostly affects people who are totally blind. As a consequence, a person’s normal sleep period is always changing. People with non-24-hour sleep-wake rhythm disorder may have insomnia symptoms and excessive daytime sleepiness when their sleep periods don’t match up with the schedule of their social and professional life.
6. Shift work disorder
This sleep disorder which is characterized by insomnia and excessive daytime sleepiness. It mostly affects people whose jobs require them to work partly or completely at night (late at night and/or early in the morning).
Most people with this disorder lose between 1 and 4 hours of sleep for each 24-hour period. Shift work disorder can be extremely dangerous. It increases the risk of accidents either at workplace or on the road. It’s believed as many as 38% of shift workers have this disorder.
7. Other circadian rhythm sleep disorders
Sleep disorders in this group are usually linked to underlying health problems. They mirror the other circadian rhythm sleep disorders listed above in terms of common symptoms, including excessive daytime sleepiness and insomnia, but people do not meet the diagnostic criteria. These are rare and unusual cases that mostly need tailored care from a sleep specialist or a doctor (2).

4. Parasomnias Such as Sleepwalking (Somnambulism), Sleep Terrors,
Sleep Enuresis, Sexsomnia etc.
Parasomnia is a sleep disorder that includes uncommon and unwanted experiences or physical events that interrupt your sleep. It can happen before sleep, during sleep or during arousal from sleep. If you have a parasomnia, you might have abnormal movements, talk, express emotions or do unusual things.
You are in fact asleep, even though your bed partner might think you’re awake. There are two different types of parasomnias, parasomnias that happen during Non-REM sleep, and parasomnias that happen during REM sleep (3).
Parasomnias that happen during Non-REM sleep include:
1. Sleep terrors
In case sleep terrors you wake up suddenly in a terrified state. You may scream or cry in fright. Sleep terrors are usually brief (30 seconds), but can last up to a few minutes. Sleep terrors are not nightmares, people are not dreaming during these episodes. Other signs of this condition are a racing heart rate, open eyes with dilated pupils, fast breathing and sweating (3).
2. Sleepwalking (somnambulism)
Somnambulism is a state of consciousness where the phenomena of sleep and wakefulness are mixed. Sleepwalking episodes usually occur in the first trimester of sleep. You usually get out of bed and walk around with your eyes wide open (you may mumble or talk (sleep talking)), leave the bedroom or sometimes even leave your home.
Therefore, there is a high risk of serious injury during this episode. Sleepwalkers often return to bed quietly on their own or with the help of someone. When you wake up, you usually don’t remember anything immediately after the episode or the next morning (3).
3. Confusional arousal
Confusional arousals and sleepwalking are very closely related conditions. Intensive panic attacks with strong restlessness, being partially awake, but confused and disoriented to time and space, vocalizations, crying and vegetative reactions are characteristic of confusional arousals.
People with this condition usually remain in bed, but may sit up, their eyes are open, and they may cry, speak slowly, have trouble understanding questions that are asked or respond in a sensible way.
The episode usually occurs during the first trimester of sleep, and may last from a few minutes to hours. Attempts by others to influence this episode of panic can lead to even greater fear and disorientation. Confusional arousals are more common in childhood, the risk of self-harm is high, and when you wake up, you usually don’t remember anything about the episode (3).
4. Sleep-related eating disorder
In the case of sleep-related eating disorder, people drink and eat while they’re partially awake. People may even eat foods they normally wouldn’t eat if they are awake (such as raw chicken or chunks of butter). However, there is a danger in this type of eating, as people may consume inedible or toxic foods, eat unhealthy or too much food. Also injuries may happen from preparing or cooking foods when only partially awake (3).
Parasomnias that happen during REM sleep include:
1. Nightmare disorder
These vivid dreams that you later remember in detail cause feelings of anxiety, fear, and terror. You may feel a threat to your dignity, survival or security. You often have trouble falling back to sleep. The risk of nightmare disorder is higher if you have stress or you experience a traumatic event, fever, some illness, major tiredness or after alcohol consumption. One and the same or similar scary content often recurs in a dream.
2. Recurrent isolated sleep paralysis
If you have recurrent isolated sleep paralysis, you can’t move your limbs or body during sleep. This occurs either before you fall asleep or as you are waking up. These episodes usually last seconds to a few minutes and are distressing, commonly causing fear or anxiety. However, sleep paralysis can be stopped if your bed partner touches you or speaks to you.
3. REM sleep behavior disorder (RSBD)
In this sleep disorder, which is more common in older adults people act out, vocalize (e.g., talk, swear, laugh, shout), or make aggressive movements (for example kicking, punching, grabbing) as a reaction to a violent dream. Many individuals with this disorder have some type of neurodegenerative disease, such as multiple system atrophy, Parkinson’s disease, stroke or Lewy body dementia (3).
Other parasomnias include:
1. Exploding head syndrome
People with exploding head syndrome hear a loud noise or explosive crashing sound in their head as they fall asleep or waking up. They may also have a sudden muscle jerk, or they may see an imaginary flash of light.
2. Sleep enuresis (bedwetting)
This kind of children and adult bedwetting occurs in children age five and older, and happens at least two times a week for at least three months.
3. Sleep-related hallucinations
People with this disorder experience hallucinations as they fall asleep or wake up. They may hear things, see things, feel things or feel movement that doesn’t really exist. They may even leave their bed to escape what they’re experiencing.
4. Sleep-related groaning (catathrenia)
With this condition, people have repeat episodes of groaning noises (long groans followed by sighs or grunts) during sleep.
5. Sexsomnia
People with sexomnia perform sexual behaviors during their sleep. These may include masturbation, sexual vocalizations, intercourse, sexual assault, or fondling your bed partner (3).

5. Sleep-Related Breathing Disorders Such as Sleep Apnea Syndrome
Sleep apnea is the most common sleep-related breathing disorder that causes nocturnal snoring or pauses in breathing, which the sleeper itself may not perceive. These symptoms make sleep intermittent and reduce the amount of oxygen in the blood. The first signs of sleep-related breathing disorders may be excessive sleepiness, daily fatigue, drowsiness, cognitive impairments, as well as memory and mood problems. Sleep apnea occurs due to blockage of the upper airway.
The risk of sleep apnea is related to obesity and the peculiarities of facial and respiratory structure. Untreated sleep apnea can in turn cause other serious health problems such as hypertension and metabolic disorders, as well as accidents at work due to drowsiness and fatigue (1).
The main types of sleep apnea are:
1. Obstructive sleep apnea (OSA)
It is the more common form of sleep apnea that happens when throat muscles relax. Usually the obstructive sleep apnea is worse during REM sleep and in the supine position (on the back). Persons with large tongue, enlarged tonsils, micrognathia, a body mass index of greater than 30, wide neck size (greater than 16 inches in women, and 17 inches in men) may be at higher risk developing this disorder. People with obstructive sleep apnea may also have an increased risk for mood disorders, hypertension, cardiovascular disease, sexual dysfunction, and memory dysfunction (4, 5).
2. Central sleep apnea
This type of sleep apnea happens when your brain doesn’t send correct signals to the muscles that control breathing. Less than 5% of sleep apnea is secondary to central sleep apnea. People with this condition might awaken with shortness of breath. They also might have difficulties getting to sleep or staying asleep. You might be at higher risk developing central sleep apnea if you are male, are older, have heart failure, use narcotic pain killers (opioid medications), or have had a stroke (4, 5).
3. Complex sleep apnea syndrome, also called as treatment-emergent central sleep apnea
This happens when someone has both obstructive sleep apnea and central sleep apnea. It is a form of sleep-related breathing disorder in which recurrent central sleep apneas (up to 5 hour) persist or appear when obstructive sleep apnea events are little by little ended with positive airway pressure. In case complex sleep apnea syndrome there is not a clear cause for the central apneas such as narcotic pain killers or heart failure (5, 6).

6. Periodic Limb Movement Disorder (PLMD), Formerly Called Sleep Myoclonus or Nocturnal Myoclonus and Restless Leg Syndrome
Complaints of periodic limb movement disorder are forced movements and strong short-term contractions of individual muscle groups, manifested as repetitive limb movements, repeated rapid twitching or shaking of the limbs. These movement problems that usually involve the lower extremities (big toe, ankle, hip, and knee), occur during sleep (most frequently in light non-REM sleep) and cause sleep disruption. In some people, the limb movements can occur in the upper extremities as well.
The causes of this disorder can vary depending on age and health status. Treatment may also vary widely, from iron supplements to specific medications. However, periodic limb movement disorder is not the same as restless leg syndrome (7).
The difference between periodic limb movement disorder (PLMD) and restless leg syndrome (RLS):
- Periodic limb movement disorder. PLMD is involuntary, and the person is usually unaware of these movements altogether. Periodic limb movements that happen during daytime can also occur, but are considered as a symptom of restless leg syndrome.
- Restless leg syndrome, also called Willis-Ekbom disease. This condition on the other hand is characterized by a voluntary response to an urge to move legs due to discomfort. For example, the symptoms of restless legs syndrome often begin in the evening, manifesting as unpleasant sensations in the legs or arms and forcing the limbs to move. Sometimes the discomfort is relieved by getting up and walking or massaging the limbs (7).

7. Narcolepsy
Narcolepsy is a chronic neurological disease characterized by an uncontrolled need for short-term sleep, which can lead to loss of consciousness (narcolepsy attack) lasting 10 to 15 minutes, in which a person falls into a deep sleep and is difficult to wake up.
People with narcolepsy often have trouble sleeping at night and, in addition, have an abnormal daytime sleep habit. Most healthy people fall asleep about an hour after falling asleep, but the REM sleep phase of many narcoleptic patients begins within a few minutes (9).
8. Cataplexy
Cataplexy is a sudden and temporary episode of muscle weakness that can range from barely noticeable relaxation of the facial muscles to complete paralysis of the muscles with postural collapse. A person experiencing cataplexy is conscious, able to breathe and move their eyes.
Symptoms of cataplexy
Symptoms of a cataplexy episode may include: twitching or grimacing of the face, unusual tongue movements, shaking of the jaw, falling of the head or jaw, tremors or bending of the knees, hanging eyelids, and speech problems. During a cataplexy attack, speech may be blurred and vision may be impaired (double vision, inability to concentrate), but hearing and awareness will remain normal. The person may also collapse completely and be immobile.
Causes of cataplexy and narcolepsy
Cataplexy is most commonly associated with narcolepsy (affecting about 70% of people with narcolepsy). Although cataplexy without narcolepsy is rare, it can also occur in other rare diseases such as Niemann-Pick type C disease, Prader-Willi syndrome and Wilson’s disease. It can sometimes be seen in other medical conditions such as stroke, multiple sclerosis, head injury and encephalitis. The symptoms of cataplexy associated with narcolepsy can start at any time. However, they often begin in childhood and adolescence, between the ages of 7 and 25.
Triggers of cataplexy
Cataplexy is usually caused by strong emotions. For example laughter, crying, fright, sudden physical exertion, surprise, or some other sudden irritation. Cataplexy attacks can occasionally occur spontaneously without the emotional trigger.
Duration of cataplexy attacks
The duration of a cataplexy attack is short, commonly lasting from a few seconds to a few minutes (usually less than 2 minutes), followed by a rapid return to normal muscle tone and function. Cataplexy seizures can be very different. They can be mild and barely noticeable (mainly involving jaw drop, weak neck and/or knee flexion) or severe – ending in a whole body collapse.
The episode passes without medical intervention. However, it is still important to make sure that the person does not hurt himself if he falls. In addition, safety measures should be put in place to prevent serious injuries due to falls. Even in the event of a complete collapse, people are usually able to avoid injury. This is because they learn to notice a sense of cataplexy approach and the fall is usually slow and progressive. When a person lies comfortably, the seizure may turn into drowsiness, hypnological hallucinations, or a sleep-inducing REM period.
Treatment of cataplexy
Cataplexy cannot be completely cured and the focus is on controlling and alleviating symptoms through good sleep hygiene practices and, if needed, medication (9, 10, 11).
Supplements For Insomnia
Here are some supplements that may help in case of insomnia. However, your sleeping problems may be caused also by some other serious health condition. Therefore, consult your doctor about how to first treat the underlying illness.
1. Melatonin
Melatonin is a hormone that your body also produces naturally, and that signals your brain that it is time to sleep. The cycle of production and release of this hormone is affected by time – melatonin levels naturally rise in the evening and fall in the morning. For this reason, melatonin supplements have become a popular sleep aid, especially in cases where the melatonin cycle is disrupted, such as due to a jet lag. According to research, melatonin helps to reduce the time it takes to fall asleep and may therefore prolong sleep and improve sleep quality (13, 14, 15).
2. Valerian
Valerian is often used as a natural remedy for the signs of anxiety, depression and menopause. It is a popular dietary supplement that can also improve sleep quality and sleep disorder symptoms in at least some people. However, more research is needed on the safety of long-term use (13, 16).
3. Magnesium Glycinate
Magnesium is a mineral that is involved in hundreds of processes in the human body and is important for brain function, as well as muscle and heart health. In addition, magnesium can help soothe both – the mind and the body, and thus promote sleep. Studies show that the relaxing effect of magnesium may be partly due to its ability to regulate melatonin production.
Magnesium also appears to increase the levels of the calming brain messenger gamma aminobutyric acid (GABA). Thus, magnesium has a relaxing effect on the body and brain, which can also help improve sleep quality (13, 17, 18, 19, 20).
4. Tryptophan (L-Tryptophan)
L-tryptophan is naturally found in animal and plant proteins and is considered an essential amino acid because our body cannot produce tryptophan itself. This amino acid is important for the development and function of many organs in the body.
After L-tryptophan is absorbed from food, part of the body converts it to 5-HTP (5-hydroxytryptophan) and then to serotonin. According to some studies, this essential amino acid can help you fall asleep faster and also improve sleep quality (13, 21, 22, 23, 24).
5. L-theanine
Daily consumption of a food supplement containing up to 400 mg of this amino acid may help to relax and improve sleep. Animal studies suggest that it may be more effective when combined with GABA (13, 25, 26).
6. Red passion flower, also known as Passiflora incarnata
The species of this popular flower involved in improving sleep originate from North America, but are now also grown in Europe, Asia, Africa and Australia. In a recent study of people with insomnia, those who took passion flower extract for 2 weeks saw a significant improvement in certain sleep parameters compared with the placebo group.
These parameters were sleep duration, sleep efficiency (i.e. the percentage of time spent sleeping compared to lying in bed) and waking time after bedtime. Thus, although further research is needed, passion flower tea or extract may help some people improve sleep quality (13, 17).
7. Ashwagandha root extract
According to a study, this natural compound with sleep-inducing potential, is well tolerated and improves sleep quality as well as sleep onset latency in people with insomnia at a dose of 300 mg extract twice daily (12).
NB! The information provided here is for informational purposes only. Therefore, do not consider it as health care or medical diagnosis and treatment. Do not consider this information as a guarantee of the results you want to achieve. In addition, this information does not replace the advice of your physician or other healthcare professional.
Even more, you should not use it to diagnose or treat a health problem. Before changing or discontinuing your existing medication, treatment, or care, or taking any dietary supplements, be sure to consult with your healthcare professional or doctor before starting any diet or program, or if you suspect you may have a medical condition.
Compiled by Maria-Helena Loik
Photos: Pexels.com, Pixabay.com, Shutterstock.com
Sources:
- Sleep Disorders | Sleep Foundation
- Circadian Rhythm Sleep Disorders – Sleep Foundation
- Parasomnias: Causes, Symptoms, Types & Management (clevelandclinic.org)
- Sleep Related Breathing Disorders » Department of Neurology » College of Medicine » University of Florida (ufl.edu)
- Sleep apnea – Symptoms and causes – Mayo Clinic
- Complex Sleep Apnea Syndrome (hindawi.com)
- Periodic Limb Movement Disorder (PLMD) (clevelandclinic.org)
- 1 in 3 adults don’t get enough sleep | CDC Online Newsroom | EduBirdie
- Narcolepsy – Wikipedia
- Wikipedia – Cataplexy
- Cataplexy: Symptoms, causes, and treatment (medicalnewstoday.com)
- Efficacy and Safety of Ashwagandha (Withania somnifera) Root Extract in Insomnia and Anxiety (nih.gov)
- 9 Natural Sleep Aids (healthline.com)
- The effectiveness of melatonin for promoting healthy sleep (nih.gov)
- Meta-Analysis: Melatonin for the Treatment of Primary Sleep Disorders (plos.org)
- Valerian for Sleep (nih.gov)
- The effect of magnesium supplementation on primary insomnia (nih.gov)
- Micronutrient Inadequacy in Short Sleep: Analysis of the NHANES 2005–2016 (nih.gov)
- The Effects of Magnesium – Melatonin – Vitamin B Complex Supplementation in Treatment of Insomnia (nih.gov)
- The Effects of Magnesium Supplementation on Subjective Anxiety and Stress (nih.gov)
- Effects of tryptophan loading on human cognition, mood, and sleep – PubMed (nih.gov)
- Side Effects and Effects Associated with the Non-Nutritional Use of Tryptophan by Humans | Oxford Academic (oup.com)
- Effects of L-tryptophan on sleepiness and on sleep – PubMed (nih.gov)
- L-TRYPTOPHAN: Uses, Side Effects, Precautions, Interactions, Dosing and Reviews (webmd.com)
- The effects of L-theanine (Suntheanine®) on objective sleep quality – PubMed (nih.gov)
- GABA and l-theanine mixture decreases sleep latency and improves NREM sleep (nih.gov)


