Low FODMAP diet is often suggested to people with IBS and GI problems to avoid carbohydrates that are hard to digest and may therefore cause symptoms. But what means FODMAP, what are low FODMAP foods and why eating these foods may be beneficial for you?
Here in this profound article you will find out all there is to know about low and high FODMAP foods, in which conditions a low FODMAP diet may be helpful, for what FODMAP stands for, and most importantly – how to implement a low FODMAP diet.
FODMAPs (Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols) are poorly absorbed sugar alcohols and short-chain carbohydrates that are hard to digest and fermented by gut bacteria in the colon. If carbohydrates don’t break down, they stay in your gut.
Even more, if there is bacterial overgrowth, the bacteria in the small intestine starts to ferment the carbs too early. All this may cause symptoms such as abdominal pain, bloating, cramping, excess gas, diarrhea and/or constipation.
Low FODMAP diet plan may be difficult to follow, as it cuts out many common and even healthy foods that may contain high FODMAPs. Certain foods are totally eliminated or extremely limited for 3-8 weeks, then gradually reintroduced into a low FODMAP diet to see if they cause symptoms.
It is not meant to be a permanent solution as it is very restrictive, but it may work well enough to be a treatment for people with gastrointestinal (GI) problems. Although there is not enough scientific evidence, it is estimated that around as much as 50% of people with IBS may benefit from a low FODMAPs diet.
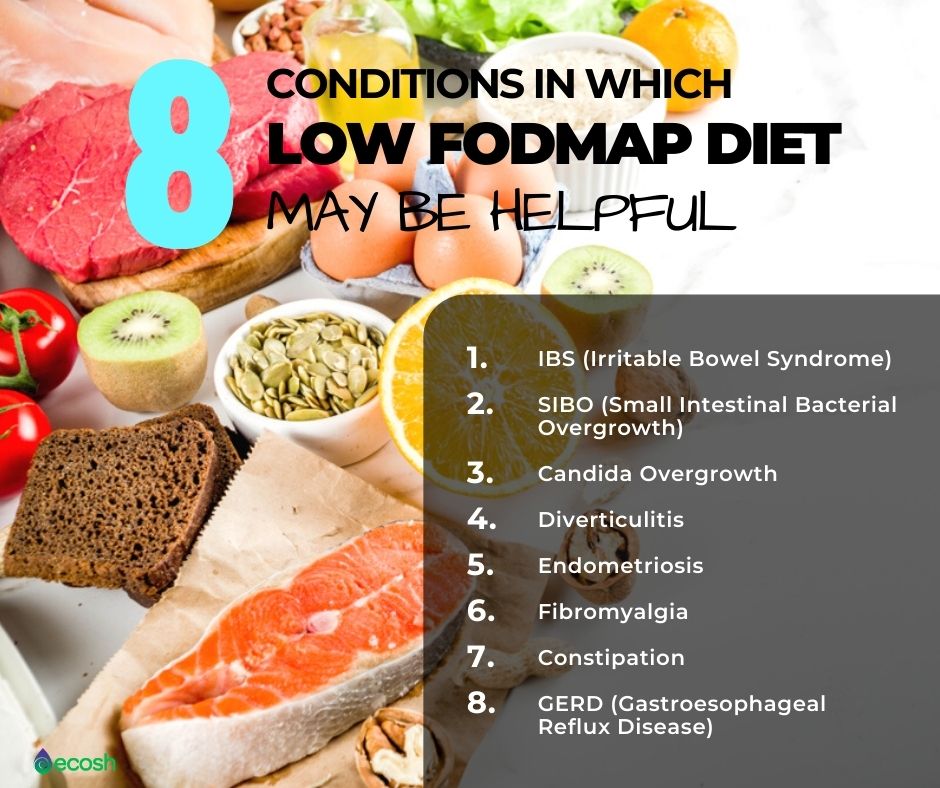
What is Low FODMAP Diet For? 8 Conditions in Which Low FODMAP Diet May be Helpful
Low FODMAP diet may be useful for many people with gastrointestinal (GI) or bacterial problems such as:
1. Low FODMAP Diet For IBS (Irritable Bowel Syndrome)
The low-FODMAP diet has been clinically proven for the treatment of IBS (irritable bowel syndrome) and related symptoms. IBS is a chronic long-term disorder that causes symptoms such as bloating, gas, cramping, abdominal pain, and diarrhea or constipation, or sometimes even both.
2. Low FODMAP Diet For SIBO (Small Intestinal Bacterial Overgrowth)
Often people who suffer from IBS also suffer from SIBO (sometimes also called blind loop syndrome). This happens when there is an anomalous increase in the general bacterial population in the small intestine (especially types of bacteria that are usually not found in that part of the digestive tract). Reducing or eliminating high FODMAP foods can improve digestive health in these people (14, 15).
3. Low FODMAP Diet For Candida Overgrowth
Some people use the GAPS, SCD or some other typical Candida diet to treat yeast overgrowth. However, according to Chris Kresser the problem with GAPS, SCD and Candida diets (depending on how they’re done) is that these may be exceptionally low-carb diets or extremely low in glucose or sugar.
But extra low-carb diets, and diets that remove every possible source of glucose or sugar in the diet – may become ketogenic. In other words, your body starts producing ketones. This is bad because there are studies according to which Candida and other yeast can actually thrive on ketones.
There are also studies, according to which white blood cells (neutrophils), are less able to kill Candida when ketones are present. Therefore, some people are starting to use a low FODMAP diet for Candida overgrowth, as it seems the bacterial markers and the fungal markers are changing and going away when implementing this diet (12).
4. Low FODMAP Diet For Diverticulitis
According to some research – a low FODMAP diet may also prevent high pressure in the colon, which, in theory, could help people correct or avoid diverticulitis (13).
5. Low FODMAP Diet For Endometriosis
Endometriosis is a long lasting disorder where tissue that is similar to the lining of the womb begins to grow in other places in your body, such as the ovaries and fallopian tubes. This condition affects approximately 1 in 9 women. Irritable bowel syndrome (IBS) and endometriosis are two disorders that have similar symptoms, such as gut pain, bloating, low grade inflammation, visceral hypersensitivity, altered bowel habits and distension.
These common features may often contribute to delay in diagnosis or misdiagnosing one condition when it’s actually the other. Women with endometriosis are more likely to have IBS. It’s also possible to have both conditions at the same time. However, when considering women with both IBS and endometriosis, eating a low FODMAP foods may assist in up to 72% of this subgroup (16).
6. Low FODMAP Diet For Fibromyalgia (FM)
Fibromyalgia is a chronic, rheumatic condition described by widespread myofascial pain that has a major impact on quality of life. This disease is linked with co-morbidities of gastrointestinal (GI) disorders and irritable bowel syndrome (IBS). According to study, a low FODMAP diet may result in a significant reduction in gastrointestinal disorders and fibromyalgia symptoms, including pain scores (17).
7. Low FODMAP Diet For Constipation
Treatments that may improve constipation in irritable bowel syndrome include following a low FODMAP diet and increasing dietary fiber intake. You can try fiber supplements such as:
- Psyllium
- Sterculia
- Linseeds
- Oats
- Oat or rice bran
- Methylcellulose
- Sterculia
8. Low FODMAP Diet For GERD (Gastroesophageal Reflux Disease)
This is a digestive condition that affects the ring of muscle between your esophagus and your stomach, and causes chest pain, burning sensation in chest, heartburn, acid indigestion, bitter taste in the mouth and dry mouth. Many people with IBS also have GERD, but not everyone who has GERD has IBS. Although there is not yet enough scientific evidence why a low FODMAP diet might help lessen GERD symptoms, many people with GERD who have tried a low FODMAP diet have reported fewer symptoms (18).
That has to be said, that although some people experience weight fluctuations as a result of restricting or expanding their food choices – a low FODMAP diet is not considered a weight loss diet.
FODMAP Subgroups Explained – What FODMAP Stands For?
FODMAP is a short term for fermentable oligosaccharides, disaccharides, monosaccharides and polyols. These are short-chain sugars (carbohydrates) that the small intestine absorbs poorly and can therefore cause digestive distress for some people.
Lets thoroughly explain all the FODMAP subgroups – exactly why they cause issues after eating and what are the food sources of each FODMAP subgroup.
O – Oligosaccharides or Oligos (Fructans and Galacto-oligosaccharide(GOS))
Oligosaccharides are a type of carbohydrate formed when 3-10 monosaccharide units (simple sugars) are linked together. They are extremely fermentable food components. These Oligos can typically cause problems for a high number of people as humans do not have the enzymes needed to break down the bonds between the chains that make up these molecules.
Also, people with IBS do not absorb oligosaccharides. That’s why eating foods high in Oligos such as beans often causes bloating, abdominal pain and flatulence. So, instead of being absorbed and used as fuel, oligosaccharides travel through the small intestine to the large intestine where they are fermented by bacteria.
This is a totally normal process, however for people with IBS, the gas that accumulates as a by-product of bacterial fermentation pushes on the walls of the large intestine and causes abdominal bloating, pain, flatulence, and altered motility (diarrhea and/or constipation).
Food Sources of Oligosaccharides
Oligosaccharides are found in a wide range of food, but they are most heavily concentrated in breads, cereals, pasta, and legumes. Nuts and vegetables are also well represented in this group, but the head-scratcher for most people is fruit, which we tend to associate with the sweeter (“M” and “P”) FODMAP categories. Oligosaccharides are water-soluble. Meaning, they will leach out liquids such as for example soup even if the food source of oligos (like garlic or onion) is removed.
- Breads and cereals such as: barley, spelt flour and kernels, white bread, wheat germ, wheat pasta,
- Vegetables such as: globe artichoke, leek, onion, garlic, Brussel sprouts
- Legumes such as: borlotti beans, adzuki beans, black beans, kidney beans, lima beans, navy beans, soybeans
- Nuts such as: almonds, cashews, pistachios
- Fruits such as: raspberries, grapefruit, dates, currants, and ripe banana
Health Benefits of Oligosaccharides
It’s extremely vital to not forget that many high FODMAP foods – particularly those in the “O” category are tremendously healthy and you should not eliminate them entirely in the long run.
Itś because fructans and galacto-oligosaccharide can act as prebiotics. These are compounds in food that promote the activity and growth of beneficial gut bacteria, especially lactobacilli and bifidobacteria. Prebiotics have many health benefits, as they:
- Promote the feeling of fullness and therefore weight loss
- Reduce antibiotic-associated and infectious diarrhea
- Boost the bioavailability and uptake of magnesium and calcium
- Help lessen the risk of colon cancer
Therefore, it’s important to test your sensitivity to foods rich in fructans and GOS during the elimination and reintroduction phases of the low FODMAP diet. After determining your personal tolerance level, you may find that you are able to incorporate small portions of foods that contain these FODMAPs into your daily diet (16, 19).

D – Disaccharide (Lactose)
This disaccharide, namely lactose, is a carbohydrate (sugar) that consists of two simple sugars (monosaccharides galactose and glucose) joined together (glycosidic bond) to create lactose, which therefore, is a di-saccharide. Lactose is found in dairy products and it requires the enzyme lactase in your body to break the bond between the two sugar molecules that are included in lactose. However, if the body is unable to produce enough lactase, lactose travels through the small intestine attracting water during this process (osmosis) and finally lands in the large intestine where it is fermented by gut bacteria.
Bacterial fermentation of undigested lactose produces excess water and the gas which pushes on the walls of the large intestine. This causes symptoms such as pain, bloating, gas, and diarrhea in people who are lactose intolerant or who malabsorb this sugar for other reasons.
For instance, some people who have the ability to make sufficient lactase are unable to do so due to some underlying condition (for example celiac disease and gastroenteritis) that damages the small intestinal villi (the source of this enzyme). Luckily, this type of secondary lactose intolerance is usually temporary, and will inverse after some time after curing the underlying problem.
Food Sources of Lactose (Also Called a “Milk Sugar”)
Lactose is found in milk products, such as:
- Cow milk
- Goats milk
- Sheep milk
- Ice cream
- Yogurt
- Sour cream
- Cheeses such as: cream cheese, Brie cheese, Camembert etc.
Fermented milk products, like kefir, yogurt and aged cheese, are lower in lactose, because bacteria added to milk during the processing of these dairy foods has a similar action as lactase (breaking down the lactose molecules into easily absorbed simple sugars).
Health Benefits of Lactose
Milk and milk products are a good source of:
- High-quality protein
- Bioavailable calcium
People who avoid dairy, should get these nutrients from other dietary sources (for example calcium-rich vegetables like collard greens, kale, or almond, hemp, quinoa or rice milk (these are all low FODMAP in appropriate serving sizes)) or supplements. However, the good news is that most people with lactose intolerance may tolerate 12 to 15g (about 1 cup (240 ml) of milk) of lactose per day (16, 19).

M – Monosaccharide (Fructose)
The smallest FODMAP carbohydrate – simple monosaccharide fructose has the ability to attract water (by a process called osmosis), as it moves through the small intestine and into the large intestine. This happens whether fructose is absorbed or not, and it can cause significant symptoms such as bloating, pain and motility issues (typically, diarrhea) for some people who are more tender to the force that this fluid applies on the intestinal walls.
Unabsorbed fructose in the small intestine goes into the large intestine and is fermented by gut bacteria. This process yields gas as a by-product which further distends the bowel, causing additional pain, bloating, and altered bowel habits in susceptible individuals.
All humans malabsorb fructose if they consume it in extremely huge amounts, and that is totally normal phenomenon. But around one-third of the population has an exceptionally limited absorption capacity and are considered to have “fructose malabsorption.” However, this is not the same as hereditary fructose intolerance (disorder that is diagnosed in infants when they start consuming formula or food that includes sucrose or fructose, and might potentially be serious).
If you want to find out if fructose might be a problem for you, you should initiate a fructose-restricted diet followed by a tolerance test (like the elimination phase and reintroduction phase of the low FODMAP diet).
This will help you discover if you are sensitive to fructose, as well as give knowledge about how much of this sugar you can eat before disturbing symptoms arise.
Food Sources of Excess Fructose
Excess fructose is mostly found in processed foods containing high fructose corn syrup (HFCS-frequently used as a sweetener), sweet foods, such as honey and fruits, but also in certain vegetables.
Luckily, many foods in this category contain a more balanced fructose-to-glucose ratio, so you can safely eat these in FODMAP friendly portions.
As many enjoyable and healthy foods contain this sugar, attempting to eliminate fructose from your diet altogether is not the best solution. Therefore try a FODMAP elimination/reintroduction protocol to find out your tolerance level for fructose.
- Excess fructose fruits:
- Apples (also contain polyols)
- Pears (also contain polyols)
- Cherries (also contain polyols)
- Mango
- Excess fructose sweeteners:
- Agave syrup light
- Agave syrup dark (also contains fructans)
- High fructose corn syrup
- Honey
- Excess fructose vegetables:
- Asparagus (also contains fructans)
- Jerusalem artichoke (also contains fructans)
- Broccoli (stalks)
- Broccolini (heads)
- Sugar snap peas
- No excess fructose fruits:
- Strawberries
- Blueberries
- Passionfruit
- Papaya
- Pineapple
- Grapes
- Orange
- Kiwi
- Clementine
- Cantaloupe
- No excess fructose sweeteners:
Fructose Health Benefits
- It carries a lower glycemic index (a measure of how carbohydrates affect blood glucose concentrations), which means it doesn’t cause a rapid rise and then a large fall in blood glucose levels.
- Fructose is 1.2 times sweeter than sucrose, which means you need to add it less during the food manufacturing process (20).

P – Polyols, Also Called Sugar Alcohols (Mannitol, Sorbitol, Xylitol, Isomalt)
Polyols are a group of versatile, reduced-calorie small-chain carbohydrates that provide sweetness and are typically used as additives in packaged foods and in sugar free foods, such as chewing gums and mints. Polyols also can be found naturally in certain vegetables and fruits.
Your body absorbs polyols via pores in the small intestinal epithelium. This happens slowly in all humans, but the rate is affected by factors such as:
- Size of the small intestinal epithelial pores
- Polyol type and dose
- Gut transit time
- The presence of intestinal disorders that reduce epithelial pore size (for example celiac disease).
Like fructose, also polyols attract water as they pass through the small intestine, which happens whether polyols are absorbed or not. This can cause motility problems (mostly diarrhea) and pain for individuals who are more sensitive to the pressure this fluid exerts on the intestinal walls. Just about all people will face digestive symptoms if they eat more than 10 – 20 grams of polyols at one time.
That is the reason why packaged foods containing mannitol or sorbitol must have a warning that states, “Excess consumption may have a laxative effect.”
Unabsorbed polyols in the small intestine go to the large intestine where they are fermented by gut bacteria. The gas produced as a by-product of this bacterial fermentation extends the bowel, and causes gastrointestinal symptoms such as bloating, additional pain, and altered bowel habits in vulnerable people if the amount consumed exceeds your absorptive capacity.
However, some polyols (particularly erythritol) are better tolerated as they are better absorbed in the small intestine. If you want to find out if polyols might be a problem for you, you can try a polyol-restricted diet followed by a tolerance test (like the elimination phase and reintroduction phase of the low FODMAP diet).
Food Sources of Excess Polyols
Polyols are mostly contained as additives in sugar-free products such as candy, chewing gum, in other low-calorie or carb-free foods, and in stone fruits and some vegetables.
- Excess polyols fruits:
- Apple (also contains excess fructose)
- Pear (also contains excess fructose)
- Cherries (also contain excess fructose)
- Apricot
- Avocado
- Blackberries
- Lychee
- Nectarine (also contain excess fructans)
- Plum (also contain excess fructans)
- Prune (also contain excess fructans)
- Excess polyols vegetables:
- Cauliflower
- Corn (sweet)
- Celery
- Sweet potatoes
- Sauerkraut (white)
- Mushrooms (Portobello, shiitake, enoki, button, dried porcini)
- candy, chewing gum, in other low-calorie or carb-free foods,
- Sugar-free products:
- Candy
- Chewing gum
- Other low-calorie or carb-free foods
A fast and efficient way to spot additional polyols in the ingredient lists of packaged foods is to search for:
Health Benefits of Polyols
Polyols may possess multiple health benefits. For instance, they are:
- Non-cariogenic (sugar-free tooth-friendly)
- Low-glycaemic (potentially helpful in diabetes and cardiovascular disease)
- Low-energy and low-insulinemic (potentially helpful in obesity)
- Low-digestible (potentially helpful in the colon)
- Osmotic (colon-hydrating, laxative and purifying) (21).

How to Implement Low FODMAP Diet? The Three Phases of The Low FODMAP Diet – Elimination Phase, Reintroduction Phase and Integration Phase
To implement FODMAP diet isn’t easy at first, as everyone’s food intolerances are different, but it’s important to remember that once you find out your food intolerances and in case IBS – the IBS trigger foods, it can be life-changing for you and you can start living a happier and healthier IBS symptom-free life.
However, being healthy doesn’t always equal following a strictly low FODMAP diet. Although, eating only low FODMAP foods may leave you feeling well, it is neither practical nor healthy. Therefore it is not wise to totally avoid certain FODMAP groups permanently if they aren’t causing any symptoms.
Note that it is better if you implement the FODMAP diet under the supervision of qualified health care professionals, like for example a registered dietician. So, let’s thoroughly explain the low FODMAP diet phases.
Low FODMAP diet phases:
- Elimination phase
- Reintroduction phase
- Integration phase
Step 1. FODMAP Diet Elimination Phase (2-6 weeks)
- Goal: The goal of elimination phase is to identify the high FODMAP foods from your present daily menu that you commonly consume, and that are provoking your IBS symptoms or symptoms of some other health condition.
- How to implement?: Firstly, see the list of the high FODMAP foods below, and switch them out for low FODMAP alternatives.
- How long does it take and when can I expect the results?: Some people start to feel better as early as after two days. However, for others, noticing results can take a few weeks. So, be patient! Overall, how long you spend time in the elimination phase should be set on in consultation with your healthcare professional, but estimatedly and usually it lasts about 2-6 weeks.
- Can I cheat in the elimination phase?: No! You should not have any cheating moments when implementing this diet. Because if you stick to it with your full commitment, the more accurate and effective the results are. Therefore, stay strong! For instance, if you are used to eating apples, swap your daily high FODMAP apple for a low FODMAP strawberries or orange (22).
Step 2. FODMAP Diet Reintroduction Phase (6-8 weeks)
- Goal: The goal of the reintroduction phase is to determine which high-FODMAP foods trigger symptoms and which do not.
- How to implement?: In this phase you gradually (one by one) reintroduce single high-FODMAP foods back into your diet. If a specific food does not cause any symptoms then you can include that specific food into your daily diet from now on. However, if it does cause symptoms – you should eliminate this food permanently.
- It’s important to remember that you should reintroduce every FODMAP subgroup (Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols) one by one while the rest of the diet remains low in FODMAPs. Sticking to this method allows you to see which FODMAP subgroups you may have intolerances to. Otherwise it will be impossible to understand what foods trigger your symptoms and all the effort goes to waste.
- How long does it take and when can I expect the results?: Usually it can take about 6 to 8 weeks to finally find out all your trigger foods. If a certain food is not suitable, you should notice it immediately or within a few days. Therefore, do not rush the process and take a break for a few days between the reintroduction of single foods, as otherwise there can be crossover effects.
This step can be the most tricky and hard to implement for people, therefore consult your healthcare professional if you need any help.
Step 3: FODMAP Diet Integration Phase (Lifelong)
- Goal: The goal of the integration phase is to establish your personalized and persistent FODMAP diet.
- How to implement?: After finding out foods that you tolerate and foods that are triggering your symptoms, you can start reintroducing FODMAPs that you were able to tolerate well and avoid only those FODMAPSs that set off your symptoms (22).
Low FODMAP Diet – Low FODMAP Foods and High FODMAP Foods
Sometimes also portion sizes can make a difference, because if you eat only extremely small amounts, there might not be enough high FODMAPs to cause you symptoms. However, it is advisable to contact your health care professional or a dietitian to make sure that you are on the right track and getting enough dietary nutrients that you can consume.
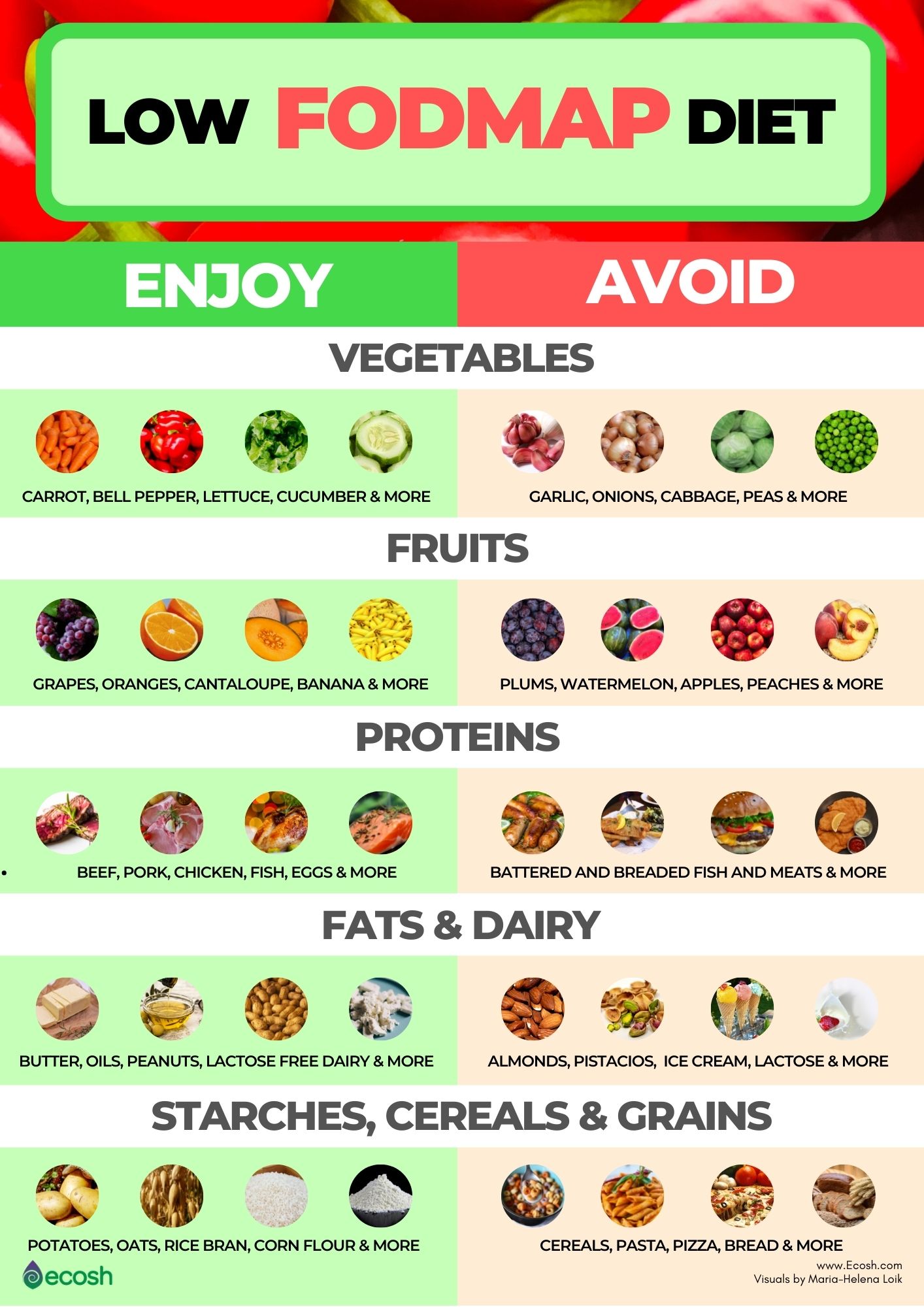
Low FODMAP Foods on a Low FODMAP Diet Include:
- Vegetables such as: alfalfa sprouts, carrot, bell pepper, bean sprouts, bok choy, green beans, lettuce, cucumber, tomato, zucchini, eggplant, bamboo shoots, ginger, olives, chives, potatoes, parsnips, and turnips.
- Fresh fruits such as: grapes, oranges, mandarins, pineapple, cantaloupe, banana, honeydew melon, blueberries, kiwi, grapefruit, lemon, strawberries, and lime.
- Protein sources such as: eggs, firm tofu, tempeh and plain cooked meats such as beef, pork, poultry, fish, seafood.
- Soy products such as: tempeh and tofu.
- Breads and cereals such as: oats, oat bran, rice, rice bran, rice cakes, corn flour, quinoa, quinoa flakes, sourdough spelled bread, corn flakes, corn pasta, spelt bread, wheat, rye and barley free breads, gluten-free bread and pasta (although gluten is not a FODMAP, many gluten-free products tend to be low in FODMAPs).
- Dairy products and alternatives: dairy products that are lactose free and hard cheeses, or ripened/matured cheeses such as lactose free milk, almond milk, coconut milk, rice milk, soy milk, brie cheese, camembert cheese, feta cheese, cheddar cheese, parmesan cheese, Swiss cheese, and mozzarella cheese. However, if you are not lactose intolerant, you may not need to avoid dairy with lactose.
- Nuts and seeds such as: peanuts, walnuts, macadamias, pumpkin seeds and pine nuts (fewer than 10-15/serving for nuts).
- Sugars, sweeteners such as: dark chocolate, maple syrup, rice malt syrup, table sugar.
- Fats such as: butter (butter is considered low FODMAP food, because the amount of lactose per serving is 1 gram or less) and oils.
- Drinks such as: fruit juice not from concentrate, water, tea and coffee (use non-dairy milk or creamers) (1, 5, 10).
High FODMAP Foods That You Should Avoid Include:
- Vegetables such as: garlic, onions, cabbage, broccoli, snow peas, green peas, sugar snap peas, cauliflower, asparagus, leeks, artichokes, lentils, beans, beetroot, sweet corn, celery, brussels sprouts, sun dried tomatoes.
- Mushrooms.
- Fruits such as (particularly “stone” fruits): apricots, peaches, plums, nectarines, prunes, mangoes, pears, apples, cherries, watermelon, avocados, blackberries and dried fruits.
- Protein sources: most legumes or pulses, some marinated meats, marinated poultry, marinated fish, sausages, some processed meats, battered fish and breaded meats and fish.
- Breads and cereals such as: all wheat, barley and rye products such as cereals, pasta, pizza, bread, snack products, biscuits and crackers.
- Dairy products and alternatives: all dairy that contains lactose such as ice cream, cows milk, soy milk (made from whole soybeans), sweetened condensed milk, evaporated milk, custard, soft cheese, yogurt, ricotta cheese, cottage cheese, and pudding.
- Nuts and seeds such as: cashews and pistachios.
- Sugars, sweeteners and artificial sweeteners such as: sugar free confectionery, sorbitol, mannitol, maltitol, xylitol, agave nectar, honey, high fructose corn syrup and isomalt (usually found in sugar-free mints and gums, and also cough syrups).
- Breadcrumbs, marinades, and sauces/gravies that may be high in FODMAPs.
- Drinks such as: fruit juice concentrate, coconut water, sports drinks and alcohol (1, 5).

If You are Suffering From IBS, Here are Some Supplements, Lifestyle Tips, and Home Remedies That May Also Help in Case IBS
Supplements for IBS
Supplements that may ease IBS symptoms include include:
- Probiotics. Good bacteria, also called probiotics, are live bacteria and yeasts that are good for you, especially for your digestive system. These good bacteria normally live in your intestines and are found in certain foods, such as buttermilk, yogurt, sauerkraut and in dietary supplements. According to recent studies, some probiotics may also ease IBS symptoms, such as bloating, diarrhea and abdominal pain.
- Fiber supplements. In case of constipation-predominant IBS you may find help from fiber supplements that contain psyllium. It activates the intestinal peristalsis, accelerates the progression of food, and induces a faster sense of a full stomach. In addition, fibers purify gut walls by binding and excreting toxins, residues, and excess cholesterol. Consuming the required amount of fiber daily helps to prevent many health problems such as obesity, irritable bowel syndrome, heart disease, diabetes, and kidney stones.
- L-Glutamine. According to study, oral glutamine supplements may safely lessen all major IBS-related symptoms (1, 9).
Lifestyle Changes, Home Remedies and Alternative Medicine for IBS
You can often control your modest signs and symptoms by making changes in your diet and lifestyle and by managing stress. Here are some suggestions for IBS relief you can try:
- Follow the IBS diet or FODMAP diet and avoid eating problem foods that may trigger your symptoms (see the full list below).
- Get enough sleep. Not sleeping enough puts your body into stress. Therefore, sleeping at least 7-8 hours a day is vital for you. If you have sleeping disorders or you suffer from insomnia, you can try practicing good sleep hygiene or take natural supplements for insomnia.
- Eat at regular times each day and do not skip meals. Eating about the same time every day helps to regulate bowel function.
- Reduce stress. Experiencing stress may make IBS worse. Therefore it’s very important to learn to manage your stress. Try yoga, meditation or whatever soothes your mind. There are very simple yoga poses for stress that can be truly helpful.
- Mindfulness and breathing exercises. Lessening your stress by practicing breathing exercises and mindfulness may also be helpful in calming down the misfiring gut nerves.
- Exercise regularly. It’s a well known fact that exercise helps lessen stress and depression, but it also stimulates normal contractions of your intestines.
- Hypnosis. Hypnosis can be effective for IBS as it can lessen abdominal pain and bloating. However, you cannot do it alone and need a trained professional who teaches you how to enter a relaxed state and then guides you in relaxing your abdominal muscles.
- Acupuncture. With IBS-C (constipation-predominant IBS), acupuncture may help relax the autonomic nervous system, which helps balance your GI tract. Acupuncture may even help people with IBS-D.
- Peppermint oil pill. According to studies, in people who have diarrhea-predominant IBS, a specifically coated pill that slowly releases peppermint oil (enteric-coated peppermint oil) in the small intestine eases urgency, bloating, pain while passing stool and abdominal pain.
Some Important Facts About IBS
- No one fully knows what causes IBS.
- Doctors do not think that in IBS it’s “all in your head”.
- IBS is not a cancer and will not lead to cancer.
- IBS is not an anatomical health problem.
- It is not a recognizable physical or chemical disorder.
- It will not lead to other gastrointestinal (GI) diseases (3).
Read more about IBS symptoms, IBS causes, risk groups, risk factors, conventional treatment and IBS diet in our previous article.
NB! The information provided here is for informational purposes only, so do not consider it as health care or medical diagnosis and treatment. Do not consider this information as a guarantee of the results you want to achieve. In addition, this information is not intended to replace the advice of your physician or other healthcare professional.
Even more, you should not use it to diagnose or treat a health problem. Before taking any dietary supplements or changing or discontinuing your existing medication, treatment, or care, be sure to consult with your healthcare professional or doctor before starting any diet or program, or if you suspect you may have a medical condition.
Written by Maria-Helena Loik
Pictures: Pexels.com, Pixabay.com, Shutterstock.com
Sources:
- Irritable bowel syndrome – Diagnosis and treatment – Mayo Clinic
- Symptoms – Irritable bowel syndrome NHS (www.nhs.uk)
- Irritable Bowel Syndrome (IBS) Causes of IBS (webmd.com)
- sorbit_intolerance.indd (gastroenterologie-ffm.de)
- Low FODMAP Diet for IBS: List of Foods to Eat and Avoid (medicinenet.com)
- Types of IBS: Symptoms, Diagnosis & Treatment (healthline.com)
- Irritable bowel syndrome: prevalence, risk factors in an adult Lebanese population | BMC Gastroenterology | Full Text (biomedcentral.com)
- 7 Natural Remedies for IBS | Everyday Health
- Randomised placebo-controlled trial of dietary glutamine supplements for postinfectious irritable bowel syndrome | Gut (bmj.com)
- Is butter lactose-free? And is butter low FODMAP? | Butter & Lactose (karlijnskitchen.com)
- Weight Management Series: How to Lose Weight on the Low FODMAP Diet – FODMAP Everyday
- Top 4 Mistakes People Make When Treating Candida Overgrowth | RHR (chriskresser.com)
- Diverticulitis Diet: A List of Foods to Avoid (healthline.com)
- SIBO Diet: Beneficial Foods and Foods to Avoid (healthline.com)
- Small intestinal bacterial overgrowth (SIBO) – Symptoms and causes – Mayo Clinic
- Endometriosis and FODMAPS (endometriosisaustralia.org)
- A low fermentable oligo-di-mono saccharides and polyols (FODMAP) diet reduced pain and improved daily life in fibromyalgia patients – PubMed (nih.gov)
- Is The Low FODMAP Diet for Me? Let’s find out! – FODMAP Everyday
- What Are Oligosaccharides? Learn All About the “O” in FODMAP! – FODMAP Everyday
- The Facts on Fructose – Calorie Control Council
- Health potential of polyols as sugar replacers, with emphasis on low glycaemic properties – PubMed (nih.gov)
- Phases of the FODMAP diet explained – Canadian Digestive Health Foundation (cdhf.ca)
- Understanding the FODMAP Diet – Canadian Digestive Health Foundation (cdhf.ca)



