Acne scars may evolve as a result of the acne healing process, and appear in the region where the acne lesion had occurred. Usually on the face, back, chest, and shoulders. Scars and skin changes caused by acne can be difficult to treat, and therefore always need professional help if you want to see real improvement.
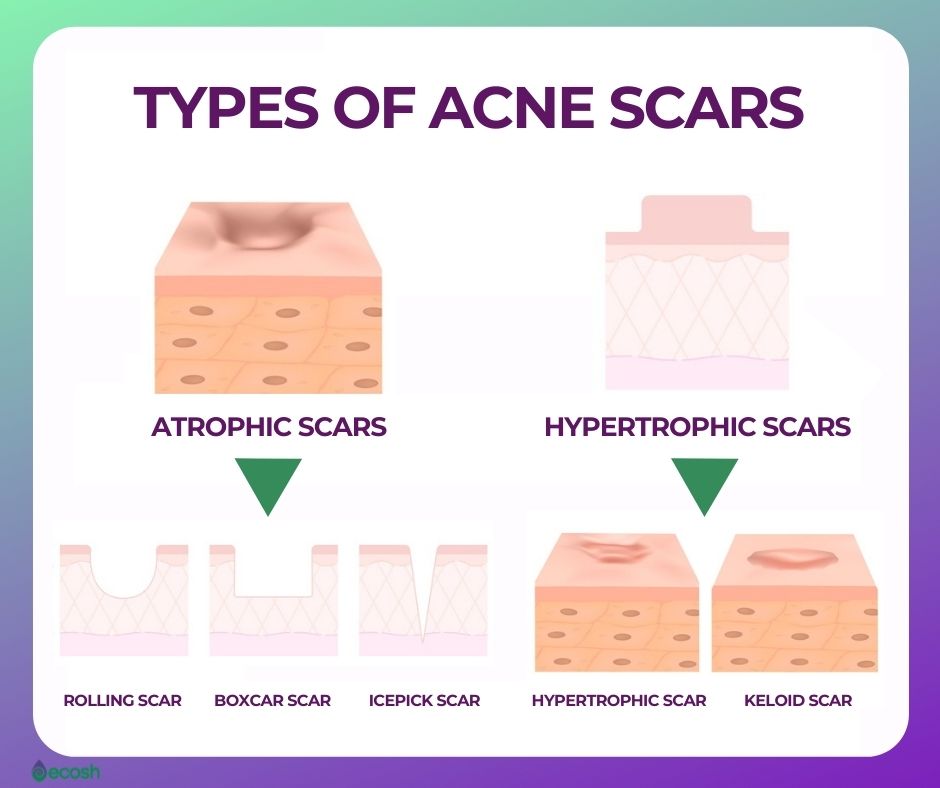
Types of acne scars include scars generated by a loss of tissue (atrophic scars, such as ice-pick scars, boxcar scars, and rolling scars), and scars generated by an excess of tissue (hypertrophic scars such as keloid scars and hypertrophic scars).
In this article, we thoroughly talk about the types of acne scars, as well as treatment options for these different types of acne scars.
Types of Acne Scars
Acne complications, such as different types of scars and skin changes can be hard to treat, and therefore always need professional help if you want to see real improvement. Below are listed the types of acne scars and other acne complications:
- Acne scars. Scarring can develop in some people as a complication of acne and last long-term after acne has healed. All types of acne spots can cause scarring, however, it’s more frequent when the most severe types of spots (nodules and cysts) burst and harm nearby skin, or if you squeeze or pick your spots.
There 2 two types of acne scars, those developed due to losing tissue and those developed due to excessive tissue.
-
- Acne scars generated by a loss of tissue (atrophic scars), such as ice-pick scars, boxcar scars, and rolling scars:
- Ice pick scars. These are small and narrow, but deep holes in the surface of your skin that look like your skin have been pierced with a sharp object, like for example ice pick.
- Boxcar scars. These are oval or round craters or depressions in the skin with steep vertical sides that are wider than ice pick scars. Due to boxcar scars, your skin may look uneven, or pitted.
- Rolling scars. This type of scarring that forms under your skin causes wave-like or rolling craters or depressions across the skin that otherwise looks normal, making it look craggy and uneven. Rolling scars aren’t as sharply defined as boxcar scars.
- Acne scars generated by an excess of tissue (hypertrophic scars), such as hypertrophic scars and keloid scars:
- Hypertrophic scars. These raised, firm scars that evolve above the surface of the skin are more frequent after a deep wound or trauma. Hypertrophic scars mostly develop on the torso (particularly in men) but can occur everywhere on the body.
- Keloid scars. These are more serious kinds of scars that rise above the skin, because in contrast to hypertonic scars – keloid scars grow larger than the original size of the wound. Even more, keloid scars may keep on growing long after the original wound itself has healed.
- Acne scars generated by a loss of tissue (atrophic scars), such as ice-pick scars, boxcar scars, and rolling scars:
- Skin damage and discoloration. After healing from acne, the affected skin may be hypopigmented (lighter), or hyperpigmented (darker) than before (1, 2, 5).

Risk Factors For Forming Acne Scars
- Your skin’s healing properties. Some people tend to scar more easily then others, so these people are the ones who may probably also evolve acne scars more easily.
- Acne severity.
- Duration. How long time passes in the middle of the beginning of acne and the first efficient treatment.
- Relapsing acne.
- Male gender.
- The severity of inflammation. There is certainly a bigger chance to develop scars if inflammation from acne continues deeper into the skin. So to lower the risk of deep inflammation and scarring, it is important to start treating acne as soon as possible.
- Squeezing and picking pimples and acne lesions. This can harm your skin and lead to an increased likelihood of skin damage, infection, and scarring.
- Smoking. As a rule, smoking leads to a higher likelihood of scarring, therefore you are more likely to also develop acne scars.
- Darker skin. Due to a variety of genetic factors, people with darker skin types have a higher chance of evolving thicker keloid and hypertrophic scars (24, 25).

Acne Scars Treatment
Atrophic Scars Treatment
Most individuals with acne scars have atrophic scars (associated with a loss of collagen) compared to hypertrophic scars and keloid scars with a ratio of 3 : 1. Sadly, there is no fast or easy topical treatment that would be efficient in raising atrophic scars that are already sunken. Therefore, it is recommended to start treating scars early before sinking while they are still red (28).
Ice Pick Scars (60%–70% Of Total Atrophic Scars) Treatment
Treatment options for ice pick scars include:
- Punch excision. In the course of this common therapy for ice pick scar treatment, your physician uses a tiny tool to cut out the scar. After cutting and removing the scar your skin around the scar is pasted back together to recover.
- Punch grafting. Physicians use this treatment method mostly for lower and larger scars. The scarred tissue will be removed like in punch excision. But in place of gluing the scar back together – the empty hole is filled with a graft of your own skin which is typically taken from behind the ear.
However, punch excision, as well as punch grafting themselves, can leave small scars. Though, these scars are much less visible, as they are flat and level with the surrounding skin.
Boxcar Scars (20%–30% Of Total Atrophic Scars) Treatment
Treatment options for boxcar scars include:
- Punch excision. Dermatologists use the same method also in the treatment of ice pick scars.
- Punch elevation. Similarly to punch excision and punch grafting, the scarred tissue will be removed. However, to soften and level off the surface of the skin, the skin at the base of the boxcar scar will be raised instead of filling the hole with a graft of your skin.
- Dermal fillers. In this fast, simple, and most routine procedure that physicians use to treat boxcar scars – dermal fillers are injected into the scar to help raise depressed areas of the skin. Dermal fillers leave scarred tissue more even with the nearby skin surface. However, the effects of this procedure are not totally permanent as they last about 18 months to 2 years.
- Laser resurfacing. There are numerous laser procedures to choose from for the treatment of acne scarring, so you should talk with your physician to determine which one would be best for you. Overall, lasers improve the surface and the color of the skin by helping to encourage collagen production and the growth of new skin tissue.
Rolling Scars (15%–25% Of All Atrophic Scars) Treatment
Subcision. This is one effective and simple surgical procedure that is done on an outpatient basis under local anesthesia. Your physician puts a needle side by side to the skin and cuts the fibrous bottom of the scar. As this fibrous base is pulling down the skin from below, cutting these bases frees scars that have become trapped in the base tissues. After the treatment when the bands have been cut, your skin should look more even and smoother.

Keloid and Hypertrophic Scar Treatments
Only a small number of people with acne (more common in darker-skinned individuals) will develop hypertrophic or keloid scars. These types of firm, raised scars are caused by excess collagen build-up that makes skin look lumpy.
Treatment for hypertrophic and keloid scars usually comes in two stages, and there are numerous different options available. First phase therapies for acne scars are aimed to lessen the height of the scar. Stage two procedures and therapies are designed to minimize skin hyperpigmentation.
All of the treatments and procedures listed here in this article should only be done by a certified professional. Moreover, these therapies may have potential side effects, such as skin peeling, burns, skin bleaching, irritation, and changes to skin texture. Therefore, consult your dermatologist to find out more about the risks and unwanted side effects involved in any procedure that you may be considering (24, 28).
1. First Stage Treatment
- Steroid injections. In this treatment, your physician injects steroids directly into the scar to thin and soften the fibrous tissue and to lower the scar’s height. To achieve the best result you may need several steroid injections spaced about 4 to 6 weeks apart.
- Cryotherapy. This is a relatively new development where liquid nitrogen is used to freeze the scar from its core, outwards.
- Dermabrasion. In this treatment, your physician works with a special tool to take off the surface of the skin through friction. This results in more flatter scars.
- Chemical Peels. In this treatment high concentrations of salicylic or glycolic acid are used to remove the outer layers of skin.
- Laser Therapy. There are two mechanisms of how these therapies work. Both (production of new collagen and/or the removal of the outer layers of your skin) results in a decrease in scar height:
- Ablative laser therapy. This treatment uses high-energy light to take off the outer layers of your skin, and at the same time stimulates the formation of the new collagen in the lower layers of your skin.
- Non-ablative laser therapy. This treatment uses heat to stimulate new collagen formation in your skin without harming the outer layer of the skin.
2. Keloid and Hypertrophic Scar Treatment (Post-Inflammatory Hyperpigmentation Treatment) – Second Stage Treatment
Luckily, in many cases, discoloration (hyperpigmentation) may often fade away all on its own over time, so you don’t have to do anything. However, if the hyperpigmentation isn’t fading, or if you have decided to help speed up the process, there are some options for you.
- Over-the-counter products. These creams that contain alpha-hydroxy acids may be good options for minor to moderate hyperpigmentation.
- Prescription topical retinoid or azelaic acid creams. These creams containing hydroquinone or vitamin C may be good options for more serious hyperpigmentation
- Dermabrasion. In this treatment, the physician uses a special tool to remove the upper layers of skin through friction (not unlike a sanding machine). Due to removing the top layers of your skin the discoloration that is caused by scarring can become lessened.
- Microneedling, also known as collagen induction therapy. In this therapy, a special tool is used to make several, mini wounds within a scar. This is made to stimulate the formation of elastin and new collagen (a protein that helps give your skin elasticity and strength) inside of the old scar with new tiny injuries (which usually heal within two days). Through this procedure, microneedling may also lessen the hyperpigmentation linked with scarring. Though reducing hyperpigmentation is not the main purpose of this treatment, so other treatments may work better for treating these types of skin problems. However, you may need multiple treatments to see benefits.
- Chemical Peels. In this treatment that can also reduce the hyperpigmentation associated with scarring – high concentrations of salicylic or glycolic acid are used to remove the outer layers of skin.
- Laser Therapy. As there are multiple laser therapies out there that can reduce scarring as well as hyperpigmentation – you should consult your dermatologist to determine which one would work best for you (5, 24, 26, 28).

Natural Treatment and Home Remedies For Acne Scars
Although there is little scientific evidence to support the efficacy of natural remedies for acne scars, some people may find some of these helpful:
- Tea tree oil
- Black seed oil (Nigella sativa)
- Rosehip seed oil
- Coconut oil
- Honey
- Turmeric powder
- Margosa (neem)
- Aloe vera
- Lemon juice
- Apple cider vinegar
- Shea butter (32, 33).
Acne Scars Prevention
Effective first-line and non-invasive options for the prevention as well as for the treatment of acne scars may include:
- Silicone-based products. Silicone-based gels, creams, and other products such as tapes may be one of the most common and effective first-line and non-invasive solutions in the prevention and also in treatment of hypertrophic acne scars and keloids.
- Steroid (cortisone) creams such as hydrocortisone. Although hydrocortisone may help lessen scarring, it is not clear whether it can also reduce acne scars, specifically (27).
Best Prevention For Acne Scars Is Acne Treatment
As there are many treatment options out there (nonprescription and prescription medications as well as therapies), each of which with its side effects and risks – you should certainly consult your doctor to find out which one would work best for you. In addition to controlling your acne, your doctor or dermatologist can also help you avoid or minimize scarring or other damage to your skin as well as make scars less noticeable.
Finding suitable treatment and finally healing from acne can take months or even years, so be patient. Below you see some of the most common acne medications, therapies, and home remedies that may be helpful for some people either alone or in combination with other medications or therapies. However, there is no warranty that any of these will work in all cases.
Topical Medications
- Retinoids and retinoid-like medications. These are gels, lotions, and creams that contain retinoic acids or tretinoin that prevent plugging of hair follicles and might therefore be helpful for moderate acne. However, these types of drugs increase your skin’s sensitivity to the sun and may lead to dry skin and redness. For example:
- Tretinoin (Retin-A, Avita, and others).
- Adapalene (Differin).
- Tazarotene (Avage, Tazorac, and others).
- Antibiotics. These kill excessive skin bacteria and lessen redness and inflammation. However, it’s not recommended to use antibiotics alone. For example:
- Clindamycin with benzoyl peroxide (Duac, Benzaclin, and others).
- Erythromycin with benzoyl peroxide (Benzamycin).
- Azelaic acid and salicylic acid. Azelaic acid (naturally occurring acid that is made by yeast) has antibacterial effects, and it may help prevent clogged hair follicles. However, it can cause mild skin irritation and skin redness. For example:
- Prescription azelaic acid (Azelex, Finacea).
- Dapsone. This is suggested for inflammatory acne, but it can cause dryness and redness. For example:
- Dapsone (Aczone) 5% gel (1).
There is no strong evidence that supports the use of aluminum chloride, sulfur, zinc, nicotinamide, resorcinol, or sulfacetamide sodium in topical acne treatments. The Food and Drug Administration (FDA) warns – that although quite rarely – some popular nonprescription acne cleansers, lotions, and other skin products can still cause a serious reaction. Therefore seek immediate medical help if after using a skin product you experience difficulty breathing, faintness, tightness of the throat, or swelling of the eyes, face, lips, or tongue (1).
Oral Medications
- Antibiotics. These are used to treat moderate to severe acne, for the shortest time possible, and usually in combination with other medications. For example:
- Tetracycline (minocycline, doxycycline).
- Macrolide (erythromycin, azithromycin).
- Combined oral contraceptives. Few of these medications are FDA approved and used for acne treatment in women who also want to use them for contraception. Side effects of these drugs include nausea, weight gain, breast tenderness, and nausea. The use of combined oral contraceptives is also linked with an increased likelihood of cervical cancer, breast cancer, and cardiovascular problems. For example:
- Drugs that combine progestin and estrogen (Yaz, Ortho Tri-Cyclen 21, and others).
- Anti-androgen agents. These work by blocking the impact of androgen hormones, but may cause painful periods and breast tenderness. For example:
- Spironolactone (Aldactone)
- Isotretinoin (derivative of vitamin A). Physicians use it if moderate or severe acne hasn’t improved with other medications. As oral isotretinoin can cause side effects such as depression, birth defects, and inflammatory bowel disease – all people receiving isotretinoin need to regularly see their doctor. For example:
- Isotretinoin (Amnesteem, Claravis, and others) (1).
Therapies
You can ask your doctor or dermatologist more information about these therapies for acne:
- Light therapy. As the bacteria that live in your skin are sensitive to specific types of light (UV) – exposure to these lights destroys the bacteria. In addition, light therapy narrows the oil glands in your skin.
- Chemical peel. In this procedure – that dermatologists use mostly for mild acne – a chemical solution (salicylic acid, glycolic acid, or retinoic acid) will be applied to your skin. Chemical peeling causes the skin to peel off and the growth of the new skin to replace it. Usually, you may need to repeat this procedure several times.
- Drainage and extraction. This means gently removing whiteheads and blackheads (comedones) or cysts with special tools such as a comedone extractor (a small pen-shaped instrument). However, this therapy gives only temporary results and may also cause scarring.
- Steroid injection. Sometimes physicians treat severe acne (nodular and cystic lesions) with steroid injection which means they inject a steroid drug directly to nodular or cystic lesions. This therapy has resulted in rapid improvement and decreased pain. Although this therapy may result in decreased pain and rapid improvement, it might also include side effects in the treated area such as discoloration and thinning of the skin (1, 6).
Self-Help Techniques, Home Remedies and Supplements For Acne
Self-Help Tips
- You should not wash or cleanse skin areas affected by acne more than twice a day. Washing your face too much, cleansing it with harsh soaps or chemicals, or scrubbing it too hard irritates your skin and can worsen acne.
- When washing the affected area, use lukewarm water, as too cold or too hot water can aggravate acne.
- For washing, use a cleanser or mild soap.
- Do not squeeze your spots. This can aggravate acne and lead to persistent scarring.
- Do not use too much cosmetics and make-up.
- If using makeup, it’s important to completely remove it as soon as possible or at least before going to bed.
- Also, do not use oil-based (comedogenic) skincare, suncare, or make-up products, as these can block your skin pores. Instead, choose water-based (non-comedogenic) products.
- In case of dry skin, select water-based and fragrance-free emollients.
- After exercise shower as soon as possible, as sweat can make your acne worse.
- Try to avoid bangs or other hairstyles in which your hair falls across your face. Also, wash your hair regularly (2).

Home Remedies
- Apple cider vinegar. Put together 1 part apple cider vinegar and 3 parts water (for sensitive skin use more water), and apply this mixture to first cleansed affected areas using for example a cotton ball. Leave it on for about 5-20 seconds, rinse with lukewarm water and gently pat dry. You can repeat this procedure 1-2 times a day (7).
- Honey and cinnamon face mask. Honey and cinnamon together may fight bacteria (P. acnes) that may have a role in causing acne one study suggests. Though it does not mean this combination cures acne, so we need more research to see whether the anti-inflammatory and antibacterial effects of honey and cinnamon may reduce pimples. To try this mask put together 2 tablespoons of honey and 1 teaspoon of cinnamon. Stir it to form a paste, and apply the mask to your cleansed face. Let it sit for about 10–15 minutes. Then rinse thoroughly and gently pat dry (13).
- Green tea. Research demonstrates that the substance epigallocatechin-3-gallate (EGCG) – which is the main antioxidant in green tea – may fight inflammation, decrease sebum production, and suppress the growth of P. acnes in people with this issue.
Numerous studies have also found that applying green tea extract to the skin notably lessens pimples and sebum production in individuals with acne (18, 19, 20, 21).
- Tea tree oil. This oil is famous for its capability to combat bacteria and alleviate skin inflammation. Also, various studies have demonstrated that applying tea tree oil to affected skin may lessen symptoms in case of mild or moderate acne. Before using, mix 1 part tea tree oil with 9 parts water. Then apply this mixture to the affected skin areas with a cotton swab. You can do this 1-2 times a day (14, 15, 16, 17).
- Witch hazel. Witch hazel contains tannins that possess powerful anti-inflammatory and antimicrobial properties which among other skin conditions (such as eczema, dandruff, burns, varicose veins, bruises, and insect bites) may also help to relieve acne. Mix 1 tbsp of witch hazel bark with 1 cup of water and soak the mixture (for example in a saucepan) for about 30 minutes. Then bring it to a boil, reduce the heat and let it gently simmer for about 10 minutes. After boiling let it sit for an extra 10 minutes, strain, and keep this liquid in a sealed box. Then apply the liquid to affected areas using a cotton ball 1–2 times a day (29, 30, 31).
Supplements
- Vitamin E, Vitamin A, and Zinc. Research indicates that individuals with acne seem to have lower levels of vitamins E, A, and zinc in their blood than individuals with clear skin. Some studies also demonstrate that taking zinc orally may have some benefits in case of acne. However, the appropriate dosage of zinc for acne has not been set, so if taking zinc do not exceed the recommended safe upper limit which is 40 mg of zinc per day (8, 9, 10, 11, 12).
- Fish oil. Fish oil contains fatty acids such as EPA and DHA and high levels of these both have been found to reduce inflammatory factors, which may also decrease the risk of acne. Some small studies have shown promising results in reducing acne by supplementing omega-3 fatty acid supplements containing both EPA and DHA daily for a long period (10 weeks). If taking omega-3 fatty acids you can follow The 2015–2020 Dietary Guidelines for Americans where the recommended dosage for healthy adults is about 250 mg of combined EPA and DHA each day (22, 23).
Acne Signs And Symptoms
Where Can Pimples Appear?
Acne can usually appear on the:
- Face. Almost all people with acne have pimples on their faces.
- Forehead.
- Upper back. More than 50% of people with acne have pimples also on the upper back and back.
- Shoulders.
- Chest. Around 15% of those with acne have pimples on their chest (2).
What Types Of Pimples Are There?
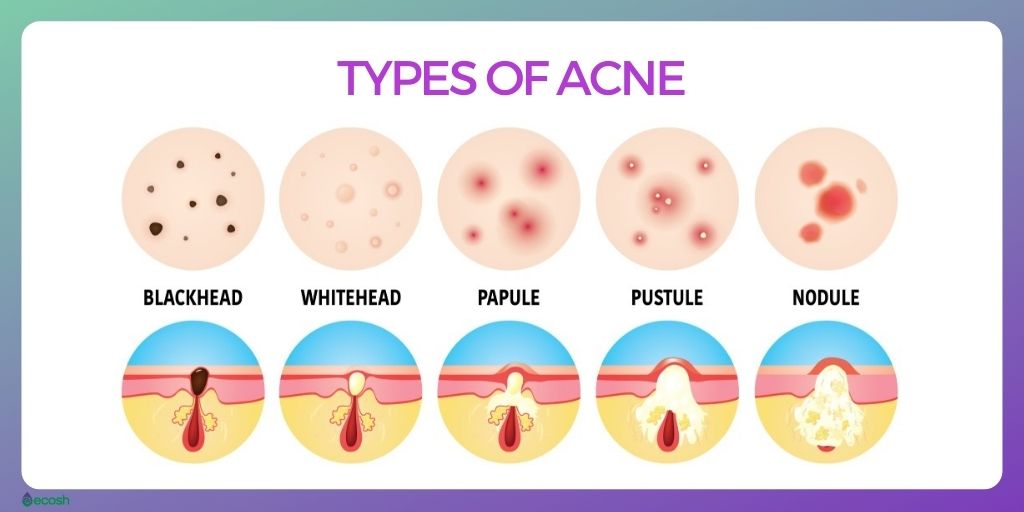
There are mostly six main types of pimples:
- Blackheads. Open clogged pores – little yellowish or black bumps that appear on the skin. Blackheads are black because the inner lining of the hair follicle produces color, or the pore is filled with oil and bacteria, which turns blackish-brown when it’s open or revealed to the air. So these bumps are not filled with dirt, as it might seem.
- Whiteheads, also called closed comedones – Closed clogged pores that look similar to blackheads, but develop when a blocked pore closes. Whiteheads may be firmer and will not empty if pressed.
- Papules. These are small red bumps, or raised areas of the skin that may feel sore or tender.
- Pustules, also called pimples – Raised red spots similar to papules but include a white tip in the center, that is caused by a build-up of pus and occurs when blocked hair follicles become infected or inflamed with bacteria.
- Nodules. These are large and hard lumps under the skin that can be painful.
- Cysts, also called cystic lesions – Large pus-filled lumps beneath the surface of your skin that look similar to boils. Cyst-like lumps under the skin are caused by inflammation and blockages deep inside hair follicles. Cysts carry the highest risk of causing permanent scarring as they are the most serious type of spot caused by acne (1, 2, 3).
What Causes Acne?
In short, acne occurs when hair follicles (small holes in your skin that an individual hair grows out of) that are connected to oil (sebaceous) glands near the surface of your skin, become blocked. And as the forehead, face, upper back, shoulders, and chest have the most oil glands, acne typically appears on these areas of your body.
The role of these sebaceous glands is to lubricate (by producing an oily substance called sebum) the hair and the skin to stop it from drying out. However, in the case of acne, these glands start to make too much of this oily substance sebum. This excessive sebum blends with dead skin cells and two of these together make up a plug in the hair follicle.
Then bacteria that live on the skin, and are usually harmless, can contaminate and infect the clogged hair follicles, leading to pustules, papules, nodules, or cystic lesions.
The Main Factors That Can Cause Acne Include:
- Bacteria
- Inflammation
- Production of excessive oil (sebum)
- Hair follicles clogged by dead skin cells and sebum (1).

Acne Risk Factors and Risk Groups
Risk Factors That May Play A Role In Triggering Or Worsening Acne Include:
- Genetics. Acne can be hereditary. So, if one or both of your parents had acne, it’s highly likely that you’ll also develop it.
- Hormones. Hormonal imbalance and changes can be major risk factors in developing acne in certain groups. For example in:
- Teenagers. Androgens (such as testosterone that plays a vital role in stimulating the growth and development of the testicles and penis in boys, and maintaining bone and muscle strength in girls) are hormones that increase in boys and girls during puberty. However, the sebaceous glands are sensitive to hormones, so they start to enlarge and make more sebum than the skin needs.
- Women. Women are at higher risk to develop adult acne than men. Its because many cases of acne in adult women are caused by the changes in hormone levels that numerous women may have at certain times. For example:
- During periods. This type of acne can last for decades, with flare-ups mostly a week before menstruation. However, the use of contraceptives usually tends to help clear up this kind of acne without any additional treatment.
- During pregnancy.
- In the case of polycystic ovary syndrome.
- Age 11 – 30. Around 95% of individuals aged 11 to 30 have acne to some extent. Girls may have it most commonly between the ages of 14 to 17, and boys between the ages of 16 to 19. Teenage acne mostly disappears if people are in their mid-20s. However, sometimes acne may extend into adult life, as around 3% of adult people have acne over the age of 35.
But, the sudden onset of severe acne in older adults may be a sign of an underlying disease that requires medical attention.
- Skin type. Individuals with darker skin types may be at higher risk to have acne complications such as scars or skin changes than individuals with lighter skin.
- Medications. For example, certain drugs that contain testosterone, lithium (used in the treatment of depression and bipolar disorder) or corticosteroids (steroids that are used in the treatment of hay fever, hives, eczema, painful joints or muscles (arthritis, tennis elbow and frozen shoulder), pain caused by an irritated or trapped nerve (sciatica), inflammatory bowel disease (Crohn’s disease), lupus, multiple sclerosis (MS), asthma, and chronic obstructive pulmonary disease (COPD)), as well as some drugs that are used in the treatment of epilepsy.
- Cosmetic products. Although acne caused by cosmetic or skincare products is now less common because the majority of products are tested and should not cause any spots (are thus claimed to be non-comedogenic) – it’s still possible that you may develop acne if your skin comes into contact with oil or too oily lotions and creams.
- Pressure of friction on your skin. If you consistently wear items that put pressure on certain affected areas of skin, for example, a backpack, cellphones, helmets, tight collars, or a headband. Even bangs can sometimes worsen acne.
- Diet. Some studies suggest that eating certain foods (for example carbohydrate-rich foods, such as bagels, bread, and chips) may also worsen acne. However, we need additional studies to see whether following a certain diet would benefit people with acne.
- Stress. Stress is not the cause of acne, but if you have acne already, stress may worsen it (1, 2, 4).

Acne Myths
There are many myths and misconceptions and myths about acne. For example:
- Poor diet, chocolate, or greasy foods lead to acne. Although an unhealthy diet, chocolate, and greasy foods are not good for anyone due to the impact they might have on your health in general – it has little or no impact on acne.
- Poor hygiene and dirty skin lead to acne. Most of these reactions that cause acne happen under the skin, not on the surface, therefore the hygiene of the skin has no impact on your acne. In fact, washing your face more than twice a day, cleansing it with harsh soaps or chemicals, or scrubbing it too hard irritates your skin and can aggravate acne.
- Skincare products and cosmetics cause acne. Most cosmetic products today do not clog pores (if you use oil-free, and non-comedogenic products), and therefore – should not worsen or cause acne if you remove makeup regularly.
- Squeezing whiteheads, blackheads, and spots helps to get rid of acne. Actually, squeezing can aggravate acne and leave you with scarring.
- Having sex influences acne. Sexual activity does not affect acne.
- Sunbathing and sun lamps improve the symptoms of acne. Up until now, there’s no decisive evidence that being more exposed to sunlight or using sunlamps or sunbeds can heal acne.
In fact, numerous medicines used in acne treatment can make the skin more sensitive to light, therefore leading to painful damage to your skin.
NB! The information provided here is for informational purposes only, so do not consider it as health care or medical diagnosis and treatment. Do not consider this information as a guarantee of the results you want to achieve. In addition, do not take this information as a replacement for the advice of your physician or other healthcare professional.
Even more, you should not use it to diagnose or treat a health problem. Before changing or discontinuing your existing medication, treatment, or care, or taking any dietary supplements, be sure to consult with your healthcare professional or doctor before starting any diet or program, or if you suspect you may have a medical condition.
Written by Maria-Helena Loik
Pictures: Pexels.com, Pixabay.com, Shutterstock.com
Sources:
- Acne – Diagnosis and treatment – Mayo Clinic
- Acne – NHS (www.nhs.uk)
- Boils – NHS (www.nhs.uk)
- Steroids – NHS (www.nhs.uk)
- Types of Scars (verywellhealth.com)
- Light Therapy (webmd.com)
- 13 Powerful Home Remedies (healthline.com)
- Evaluation of serum vitamins A and E and zinc levels according to the severity of acne – PubMed (nih.gov)
- The safety and efficacy of zinc gluconate in the treatment of acne – (nih.gov)
- Zinc therapy in dermatology (nih.gov)
- Effects of oral zinc and vitamin A in acne (nih.gov)
- Comparison of oral treatment with zinc sulfate and placebo in acne – Wiley Online Library
- Antibacterial Activity of Ethanolic Extract of Cinnamon Bark, and Honey (nih.gov)
- Tea tree oil gel for mild to moderate pimples (nih.gov)
- Treatment of acne with a combination of tea tree oil, and Aloe vera (nih.gov)
- New Perspectives on Antiacne Plant Drugs (nih.gov)
- Applications of tea tree oil in dermatology (nih.gov)
- Epigallocatechin-3-gallate improves acne in humans (nih.gov)
- The effects of topical green tea and lotus on facial sebum (nih.gov)
- Oral aqueous green tea extract and acne vulgaris (tbzmed.ac.ir)
- The effects of green tea on acne vulgaris – Wiley Online Library
- Dynamics of the human skin mediator lipidome in response to dietary ω-3 fatty acid supplementation (nih.gov)
- Effect of dietary supplementation with omega-3 fatty acid and gamma-linolenic acid on acne (nih.gov)
- Keloid and Hypertrophic Scars – acne support
- Prevalence and Risk Factors of Acne Scarring Among Patients Consulting Dermatologists in the USA (nih.gov)
- Hydrocortisone for acne (medicalnewstoday.com)
- Can Silicone Gel Help Treat Acne Scars? (newgelplus.com)
- Intralesional cryotherapy for hypertrophic scars (nih.gov)
- Efficacy of over-the-counter skincare regimen for acne (nih.gov)
- Inhibition of Staphylococcal Pathogenesis by Witch-Hazel and Green Tea Extracts (nih.gov)
- Medicinal plants used in treatment of inflammatory skin diseases (nih.gov)
- 5 Natural Remedies For Acne Scars (healthline.com)
- How Do You Get Rid of Acne Scars Naturally? (medicinenet.com)



“The depth of analysis in this blog post is impressive. It’s refreshing to find a resource that not only educates but also inspires action. The clear writing style and thoughtful explanations make complex concepts accessible. Keep up the great work!”